Case study: Monitoring phrenic nerve paresis with POCUS after regional anesthesia
A 52-year-old male patient with a long-standing history of chronic shoulder dislocations presented for elective arthroscopic shoulder surgery. Given his history of recurrent shoulder instability, the surgical team anticipated significant postoperative pain, leading them to plan an interscalene brachial plexus block for postoperative analgesia. This type of block, frequently used for shoulder surgery, is known for its effective pain relief by anesthetizing the nerves that supply the shoulder. However, a common side effect of the interscalene block is phrenic nerve paresis, which can result in diaphragmatic dysfunction or paralysis.
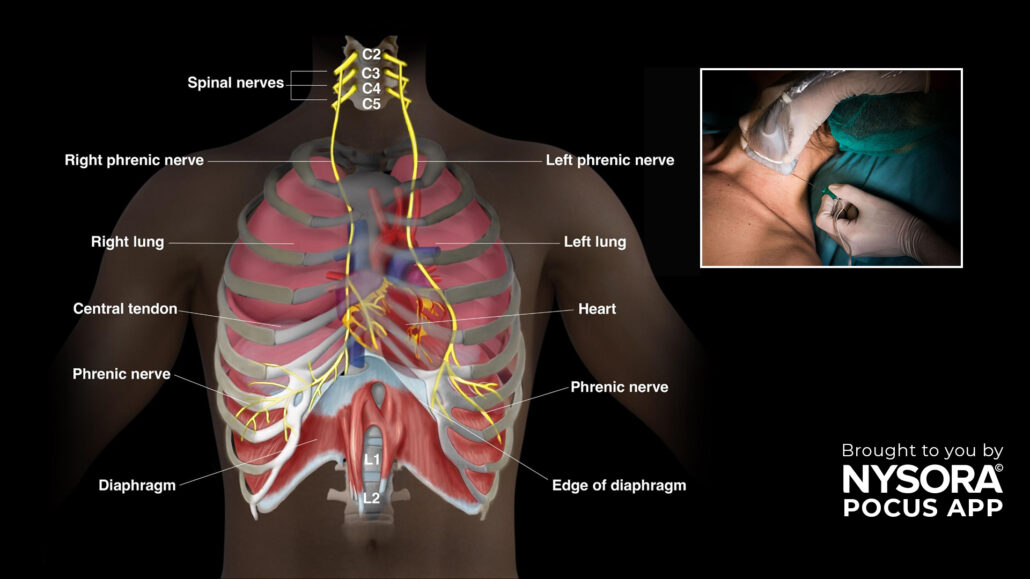
Understanding phrenic nerve paresis
The phrenic nerve is responsible for innervating the diaphragm, the main muscle involved in breathing. Because of the close anatomical relationship between the phrenic nerve and the interscalene space, there is a significant risk that the nerve could be affected during the block, resulting in diaphragmatic paralysis. This complication, while typically temporary, can reduce the patient’s respiratory capacity and lead to discomfort, especially in patients with pre-existing lung conditions or obesity.

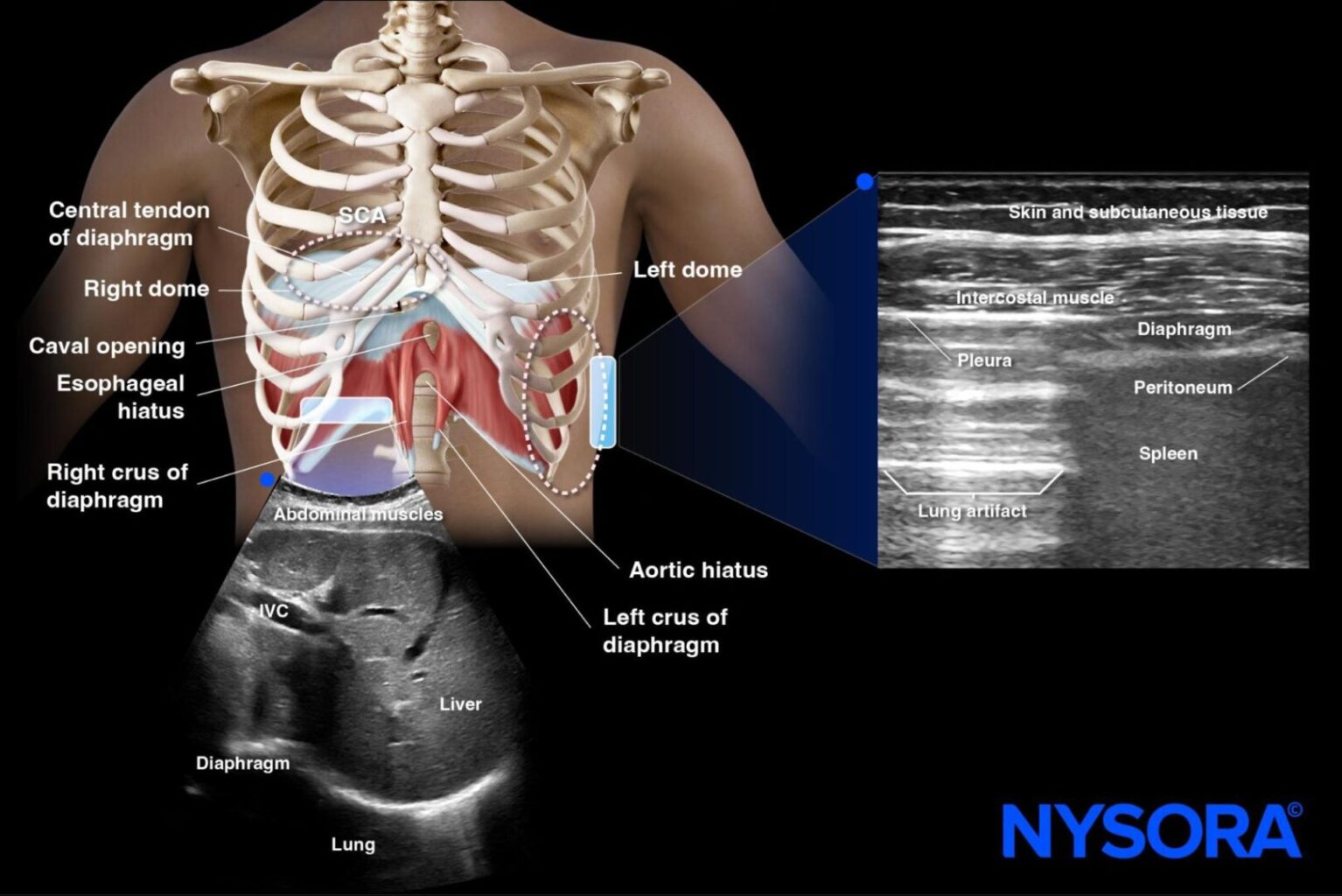
In this case, to proactively manage the risk of respiratory complications, point-of-care ultrasound (POCUS) was used to monitor the patient’s diaphragm function before and after the block.
Preoperative diaphragm assessment
Before the block was administered, the anesthesia team used diaphragm ultrasound to assess the baseline function of the diaphragm. The subcostal view was selected as the primary scanning window, which allows for clear visualization of the diaphragmatic excursion (the movement of the diaphragm during the respiratory cycle).
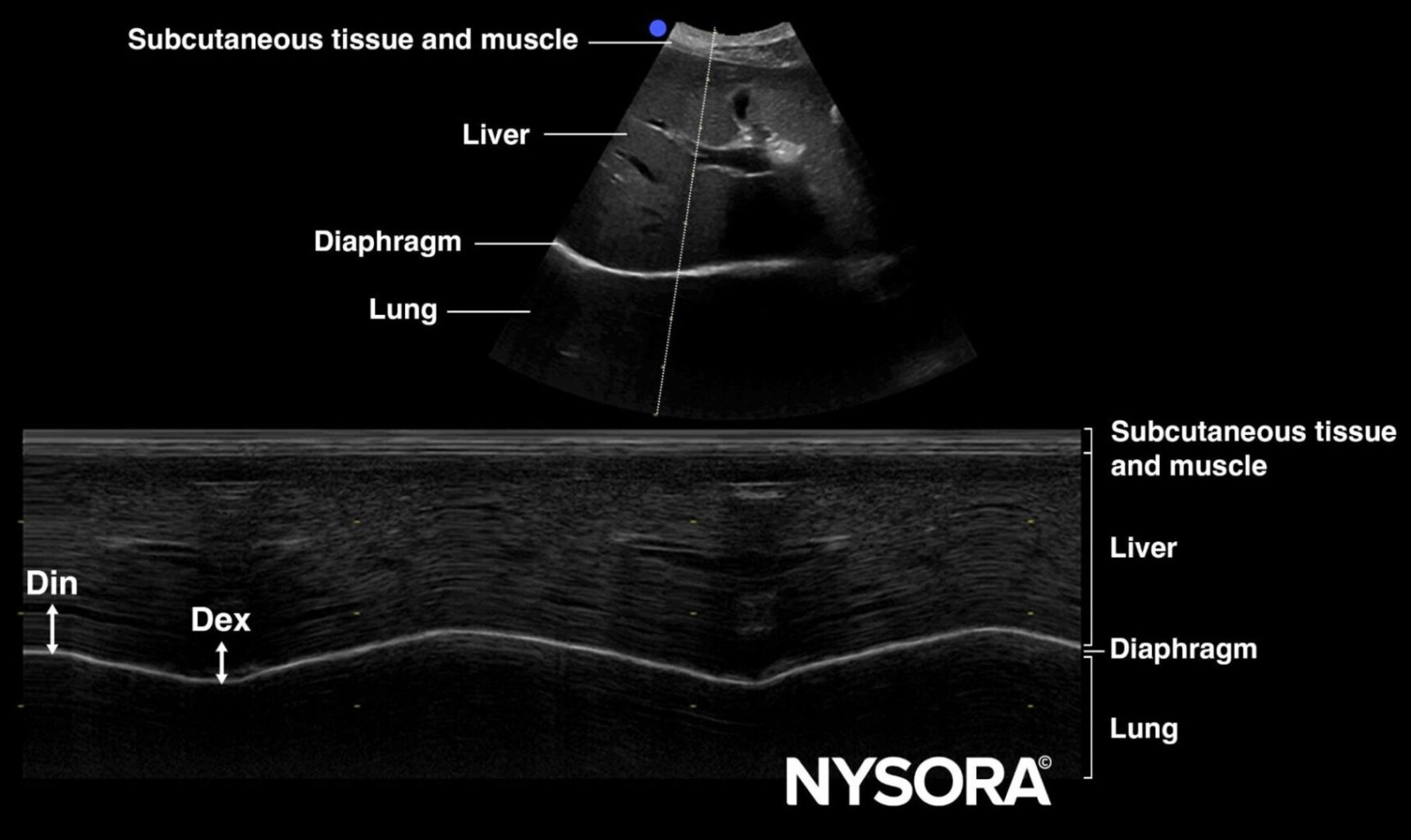
- Baseline observation: Pre-block, excursions of 1 cm were measured during shallow breathing, indicating that the patient’s diaphragm was functioning properly. This baseline measurement is crucial for comparison with postoperative function to identify any potential changes.
Postoperative diaphragm monitoring
Following the administration of the interscalene block and the successful completion of surgery, POCUS was again utilized to assess any changes in diaphragmatic function.
Post-block, the ultrasound revealed a reduction in diaphragmatic excursion, a hallmark sign of phrenic nerve involvement.
- Measured excursion: During shallow breathing, the patient’s diaphragm moved only 0.8 cm during shallow breathing, significantly lower than the expected range for a healthy individual, which is typically around 1.0 cm (during shallow breathing). This confirmed partial diaphragm paralysis.
Clinical Implications
Although phrenic nerve paresis is a known and expected side effect of the interscalene block, continuous monitoring through ultrasound is essential to ensure the extent of paralysis does not lead to significant respiratory compromise.
In this case, while the diaphragmatic movement was reduced, the patient remained asymptomatic, with no noticeable shortness of breath or respiratory distress. The close monitoring allowed the medical team to confidently manage the patient’s respiratory status without the need for additional interventions.
Patient Outcome and Management
Despite the measured reduction in diaphragmatic excursion, the patient tolerated the block well and exhibited no respiratory symptoms during the postoperative period. The anesthesia team continued to monitor the patient using POCUS, confirming that the diaphragm’s function began to normalize within 24-48 hours, consistent with the expected temporary nature of phrenic nerve paresis following interscalene blocks.
By utilizing POCUS, the anesthesia team was able to:
- Confirm diaphragmatic dysfunction early.
- Avoid unnecessary interventions, such as supplemental oxygen or more invasive monitoring.
- Ensure patient safety through continuous, real-time evaluation.
This case demonstrates how POCUS is an invaluable tool in regional anesthesia, providing a rapid, accurate, and non-invasive method for monitoring diaphragmatic function.
Transform Your Practice with POCUS
Incorporating diaphragm ultrasound into your clinical practice can significantly enhance your diagnostic capabilities, particularly in regional anesthesia where phrenic nerve involvement is common. POCUS offers the ability to monitor, diagnose, and intervene early in cases of diaphragm dysfunction, ensuring optimal patient care and safety.
Download the NYSORA POCUS App today to learn these essential skills and more. Empower your practice with the most advanced ultrasound techniques and provide exceptional care for your patients.




