
Case study:The SHAC technique for treating adhesive capsulitis
Adhesive capsulitis, more commonly known as frozen shoulder, is a debilitating condition that causes pain, stiffness, and a significant loss of shoulder mobility. For many patients, traditional treatment methods can be slow to bring relief, and the journey to recovery is often fraught with setbacks. However, a novel ultrasound-guided approach, known as the Saline Hydrodistension of the Anterior Capsular (SHAC) technique, is emerging in the treatment of this condition.
Understanding adhesive capsulitis
Adhesive capsulitis is characterized by the formation of excessive scar tissue within the shoulder joint, leading to painful restriction of movement. The condition can be primary, occurring spontaneously, or secondary, often following trauma, surgery, or other underlying health conditions. Patients with this condition typically endure months of pain and a gradual loss of both active and passive range of motion.
What is the SHAC technique?
The SHAC technique represents a significant advancement in the management of adhesive capsulitis. This procedure involves the precise injection of saline and steroids into the anterior capsular space of the shoulder joint under ultrasound guidance. Unlike more traditional methods, such as posterior or rotator interval approaches, the SHAC technique offers targeted pain relief and allows for immediate mobilization of the shoulder post-procedure.
How does the SHAC technique work?
Anatomy and access points
The SHAC technique leverages specific anatomical landmarks within the shoulder joint:
- Fascial sheaths: The procedure targets the fascial sheath between the deltoid and subscapularis muscles, as well as the sheath beneath the subscapularis myotendinous junction. These sheaths provide optimal access to the glenohumeral joint.
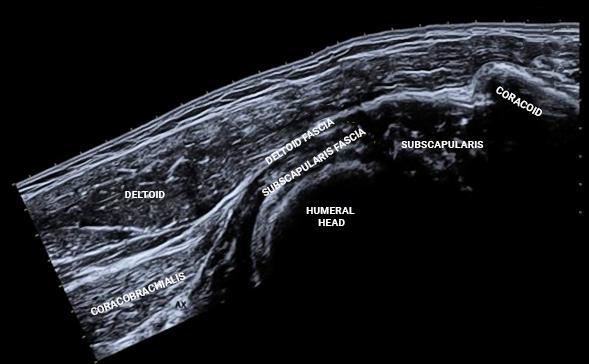
Ultrasound anatomy of the fascial sheaths providing access to the glenohumeral joint (Adapted from Galluccio et al., 2021).
- Foramen of Weitbrecht: Located between the superior and middle glenohumeral ligaments, this foramen allows entry into the intra-articular space.
- Foramen of Rouviere: Another access point, located between the middle and inferior glenohumeral ligaments, offers an alternative route into the joint.
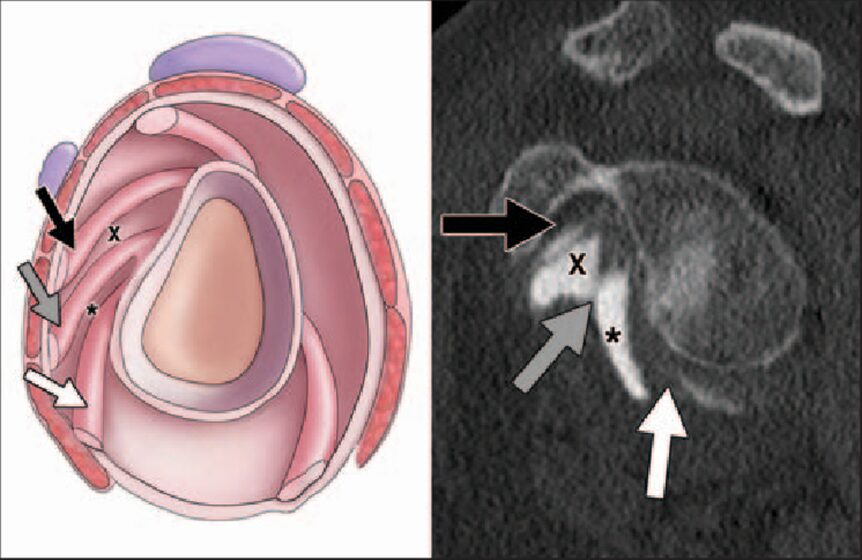
Sagittal drawing (left) and corresponding sagittal MDCT arthrographic image (right) of normal glenohumeral anatomy show superior glenohumeral ligament (black arrow), middle glenohumeral ligament (gray arrow), anterior band of inferior glenohumeral ligament (white arrow), and communications of subscapularis recess and glenohumeral joint proper through foramen of Weitbrecht (X), which is located between superior and middle glenohumeral ligaments or through foramen of Rouviere (asterisk), which is located between middle and inferior ligaments. (Fritz et al., 2012)
The procedure
The SHAC technique is performed with the patient positioned supine, with the arm extended and maximally externally rotated. Using a high-frequency linear ultrasound transducer, the physician visualizes the relevant structures and guides a needle into the anterior capsular space beneath the subscapularis muscle.
Once in place, the physician injects a small amount of lidocaine to anesthetize the area, followed by 40-50 mL of sterile saline. The saline is introduced in 10 mL aliquots, gradually distending the joint capsule. The procedure concludes with the injection of a corticosteroid, such as triamcinolone, to reduce inflammation and further alleviate pain.
Why choose SHAC?
The SHAC technique offers several unique advantages:
- Targeted pain relief: By focusing on the pericapsular space, SHAC effectively targets the terminal articular branches of the suprascapular and axillary nerves, providing superior analgesia.
- Immediate mobilization: Unlike other techniques, SHAC allows for immediate post-procedure mobilization, which is critical in preventing further stiffness and promoting recovery.
- Alternative to nerve blocks: This technique can be a valuable alternative when nerve blocks are technically challenging or when patients are unable to tolerate certain positions.
- No complex positioning: The SHAC technique does not require the complex positioning that some other techniques demand, making it more accessible and less stressful for patients.
Case example
Consider the case of a 62-year-old man who had been struggling with persistent shoulder pain for six months. Traditional therapies had provided little relief, and his range of motion had become severely restricted. After undergoing the SHAC technique, the patient experienced a 90% reduction in pain within just seven days. Additionally, 80% of his shoulder’s range of motion was restored, allowing him to return to his normal activities with minimal discomfort.

Post-procedure care and recovery
After the SHAC procedure, patients are advised to rest and apply ice to the injection site. Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended for the first few days to manage any residual pain or inflammation. Importantly, patients should begin physiotherapy and home exercises immediately to maintain the improvements in mobility and to prevent recurrence of stiffness. A follow-up visit is typically scheduled within five days to monitor progress and make any necessary adjustments to the treatment plan.
Conclusion
The SHAC technique is a novel technique in the treatment of adhesive capsulitis. Its ability to provide targeted pain relief, combined with the potential for immediate mobilization, makes it an attractive option for patients and healthcare providers alike.
References
- Galluccio F, Fajardo Perez M, Yamak Altinpulluk E, Hou JD, Lin JA. Evaluation of Interfascial Plane and Pericapsular Nerve Blocks to the Shoulder Joint: A Preliminary Analysis of Shoulder Anterior Capsular Block. Pain Ther. 2021;10(2):1741-1754.
- Fritz J, Fishman EK, Small KM, et al. MDCT arthrography of the shoulder with datasets of isotropic resolution: indications, technique, and applications. AJR Am J Roentgenol. 2012;198(3):635-646.
For more detailed information on this case and how Dr. Madhan Pandian diagnosed and treated this patient, download NYSORA’s US Pain app!




