So, you’re expecting. Congratulations! Crossing the threshold into motherhood can be accompanied by a rational dose of fear, despite the euphoria of entering such an exciting new chapter of your life – but what should you know when it comes to the nitty-gritty of it all, just moments before you meet that special little one?
Science has been advancing rapidly throughout the years, and all things aside, we’re lucky to live in a time where doctors use evidence-based knowledge to make informed decisions on what to do and when to do it. What better proof do we need than these compelling stats: From 1990 to 2015, death during childbirth has dropped by 56.9% worldwide (Roser & Ritchie, 2015). That figure is reassuring on its own, but it isn’t only that which proves the efficacy and importance of modern medicine during labor. We must take into consideration the impact of modern medicine in reducing pain and stress during this magical (albeit a bit messy) experience, and for this, we present to you our perspective of one of the most efficient methods in pain control – the epidural.
What’s an epidural?
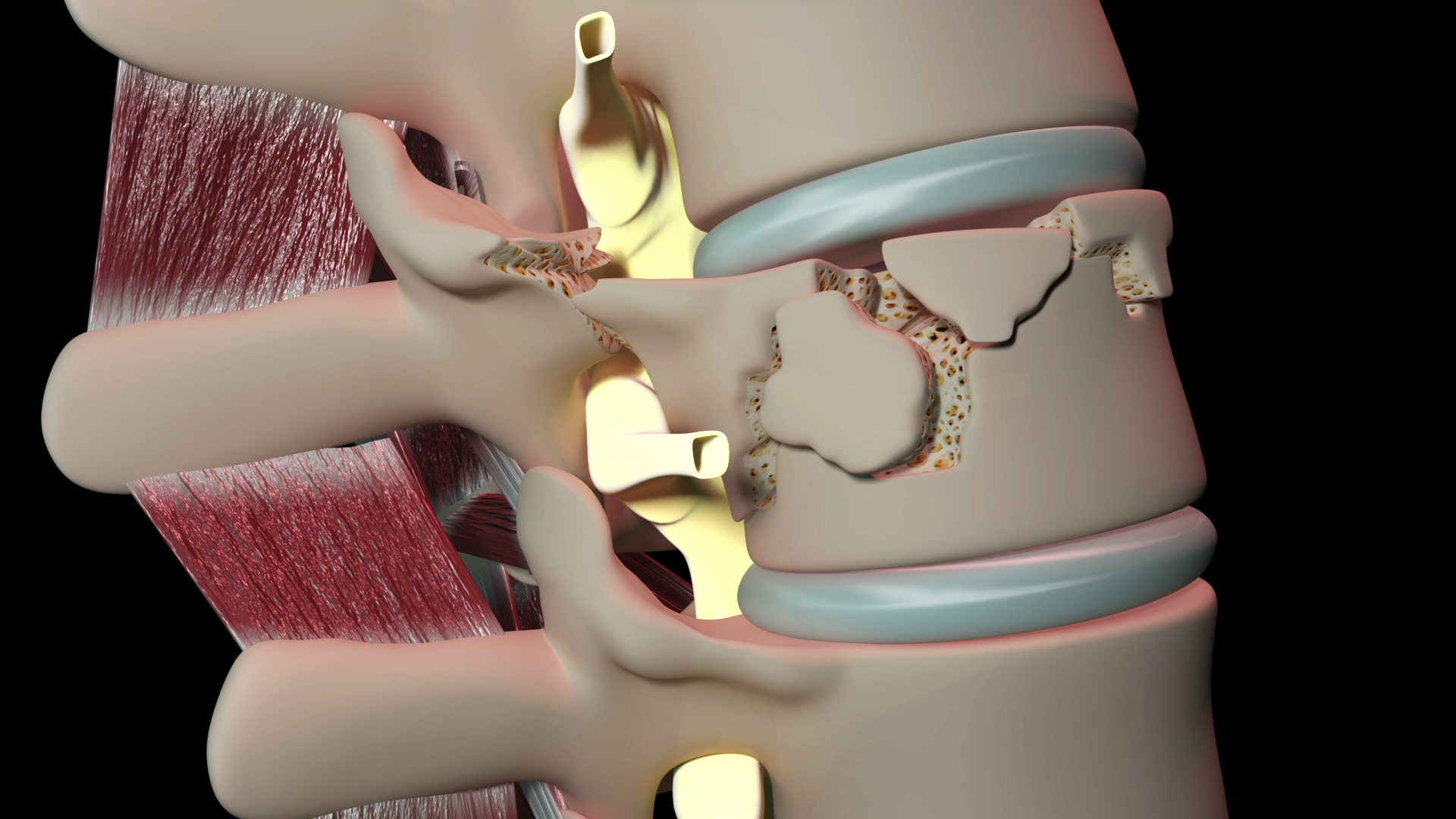
An epidural is an anesthetic agent used most commonly for childbirth to alleviate pain throughout the lower body. Here’s an interesting historical fact: It was initially coined in the 1850s! However, it took nearly a century to develop into a suitable method to assist women in labor. Labor, of course, isn’t the only function of this highly potent anesthetic – it’s also used for things like hernias, chronic postoperative pain, and other spinal injuries. When it comes down to it, an epidural serves to inject medicine that then blocks the nerves in our body that send signals to our pain receptors, leaving us comfortably numb rather than writhing in pain. A (to be honest, fairly large) needle is injected into the “epidural space” around the spinal cord’s vertebrae.
This is then most often attached to a catheter which can then pump in the necessary amount of the required substances. Keep in mind, if you’re being offered an epidural, it means that the medical professionals around you are confident that it will only benefit your experience. Basically, an epidural is a feeding tube into your spine that allows for more control when dosing you with the necessary meds to keep you comfortable.
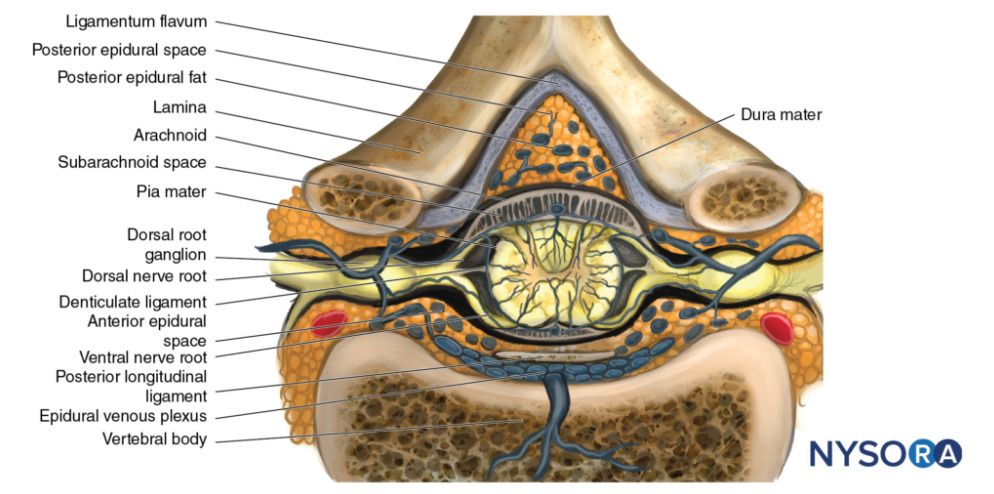
Cross-sectional view of the spinal cord depicting the ligamentum flavum in respect to the posterior epidural space.
This aside, there are a couple of different ways to administer your epidural, depending on your circumstances. Generally speaking, you’ll either be given an epidural catheter or a spinal injection. What’s the difference in practice, you might ask? We consider that a catheter in medicine usually means more moment-to-moment flexibility when it comes to dosing. Your doctor can evaluate the situation as seconds go by and adjust your dosage accordingly, making sure you get exactly as much as you need. A spinal injection, on the other hand, is a straight-up injection into the epidural space that takes effect quickly, but wears off pretty quickly too. What doctors will often do is give their patients a spinal injection right at the start to be able to painlessly insert the catheter and then keep up the analgesia throughout the procedure. This combination has been referred to as a “walking epidural” since it isn’t as completely numbing and allows you to move around a bit more than you would ordinarily be able to.
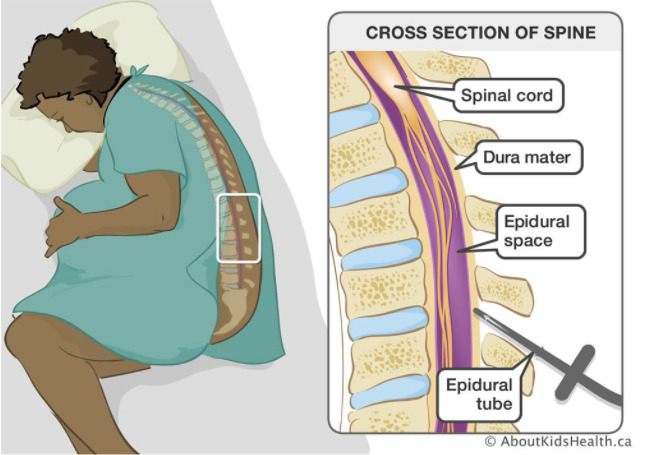
Cross-sectional view of the spine.
What do doctors have to say about it?
In general, obstetrician-gynecologists (OB-GYNs) and anesthesiologists boast a very positive outlook on epidural analgesia during the birthing process. It aids to dodge the need for cesarean deliveries (c-sections) and brings about a much more pleasant experience than the all-natural alternative. There are certain risk factors of course, as with anything, that doctors closely monitor and ensure will not pose a problem before even mentioning the epidural to you. Years of experience have prepared them for you to arrive at their table, and your best interest is their best interest – after all, what else do doctors aim to achieve if not the livelihood of their patients?
A common issue faced by doctors in discussions with future moms is that of the external pressures put on these women before they discuss their options with their doctors. There is a strange social pressure put onto women to sacrifice their comfort in any possible way for the sake of motherhood, even if one may have nothing to do with the other. Going through the birthing process without using the tools offered to ease your journey does not offer any genuine rewards, nor does it change many of the postpartum symptoms such as headaches and drowsiness. The result is the same, it is only the actual procedure that leads up to it that changes.
A third of mothers-to-be decide against getting an epidural for this or that reason, but doctors commonly bring up that social pressure by family, friends, or media leaves the biggest impact. Misinformation and misconstrued stories divert women from easing their pain, believing that the cons outweigh the pros. Doctors often have to spend extensive amounts of time persuading these women to follow the standard, modern medical procedures, and often don’t even succeed by the end of it all. For the medical professionals involved, this lack of trust poses an obstacle for completing their work without a hitch and more often than not leaves both the doctor and the patient exhausted by the end of the ordeal.
But what about you and your little one?
Trully, the epidural is a miracle of modern medicine when it comes to the struggle of labor. The worst of it all is the whole 10 seconds of pinching sensation while you receive a local anesthetic at the spot where your catheter will be administered; after these ten seconds, you’re home free and clear as a bell – which must be said is another benefit of the epidural. No fuzziness or drowsiness comes out of it, and you’re conscious and alert for the whole baby-birthing event. It’s certainly a much more soothing and elegant experience than natural childbirth, with its accompanying heaving and pushing and severe pain.

Furthermore, unlike a few other pain-controlling substances, it’s been proven through numerous scientific sources and many, many epidural labors that the epidural poses no risk to your newborn – so rest easy!
Is there a downside?
The common side effects of the epidural, all in all, are pretty much just slight discomforts. Things like not actually being able to actively move around or feel your legs while this all is going on, and thus not really being able to feel how hard you’re pushing – childbirths that use an epidural have been shown to last about two hours longer than natural births on average, particularly if you’re having your first.
For the sake of honesty and making a completely educated decision, it is worth mentioning that at most 0.0004% of women develop some form of permanent nerve damage after their epidural. Besides this, it isn’t uncommon to have swelling or bruising around the administration site, and about 1 in 200 women experience headaches later on.

In any case, whether or not you chose to get an epidural is up to you and your doctor – all that you can do is be as informed as possible, and remember that any pressure for the self-sacrifice of natural birth is just that – pressure. All that should impact your decision are the benefits and downsides that are totally circumstantial, and completely based on your individual background.