Learning objectives
- Describe the underlying mechanisms of AR
- Recognize the symptoms of AR
- Manage patients with AR
Definition & mechanisms
- Aortic regurgitation (AR) is defined as diastolic reversal of blood flow from the aorta into the left ventricle
- Most common etiology: Atherosclerotic degeneration of the valve, especially in the presence of a bicuspid aortic valve
- Acute AR:
- May develop from:
- Valvular abnormalities (most commonly infective endocarditis)
- Aortic abnormalities (mostly aortic dissection)
- Iatrogenic causes such as traumatic injury (i.e., motor vehicle accident) or during transcutaneous aortic valve procedures
- Characterized by an abrupt increase in left ventricular end-diastolic volume
- In severe cases, patients often present with pulmonary edema and even cardiogenic shock
- May develop from:
- Chronic AR:
- Most commonly caused by atherosclerotic degeneration of the valve and/or congenital bicuspid aortic valve
- In the early phases, compensatory mechanisms keep the left ventricular ejection fraction in the normal range
- Over time, the LV dilates and hypertrophies to normalize wall stress by maintaining the ratio of ventricular wall thickness to cavity radius
- Compensatory mechanisms allow patients to remain stable and asymptomatic for many years, even in the presence of severe AR
- If wall thickening fails to keep up with the volume overload, there is an increase in wall stress which then results in a reduction in LV systolic function and LVEF due to myocyte damage
- As LV filling pressures rise, symptoms of fatigue and dyspnea may appear
- Angina can develop even in the presence of normal coronary arteries
- Pulmonary edema and heart failure can occur due to chronically elevated left-sided filling pressures
Signs & symptoms
- Symptoms
- Chronic AR
- Patients with chronic AR remain asymptomatic for years. When symptoms appear, they are due to left heart failure:
- Chest pain
- Increasing exercise intolerance
- Dyspnea
- Paroxysmal nocturnal dyspnea
- Orthopnea
- Patients with chronic AR remain asymptomatic for years. When symptoms appear, they are due to left heart failure:
- Acute AR
- Because of a lack of chronic compensation, patients usually present with pulmonary edema and heart failure refractory to optimal medical therapy
- Patients are often hypotensive and clinically appear to be on the verge of cardiovascular collapse
- Chronic AR
- Diagnostic signs
- Collapsing pulse and wide pulse pressure
- Displaced apex inferolaterally
- Early diastolic high-pitched murmur
- An Austin-Flint murmur may be heard in mid-diastole at the apex
- De Musset’s sign – Head nodding with each pulse
- Corrigan’s sign – Visible carotid pulsation
Severity assessment
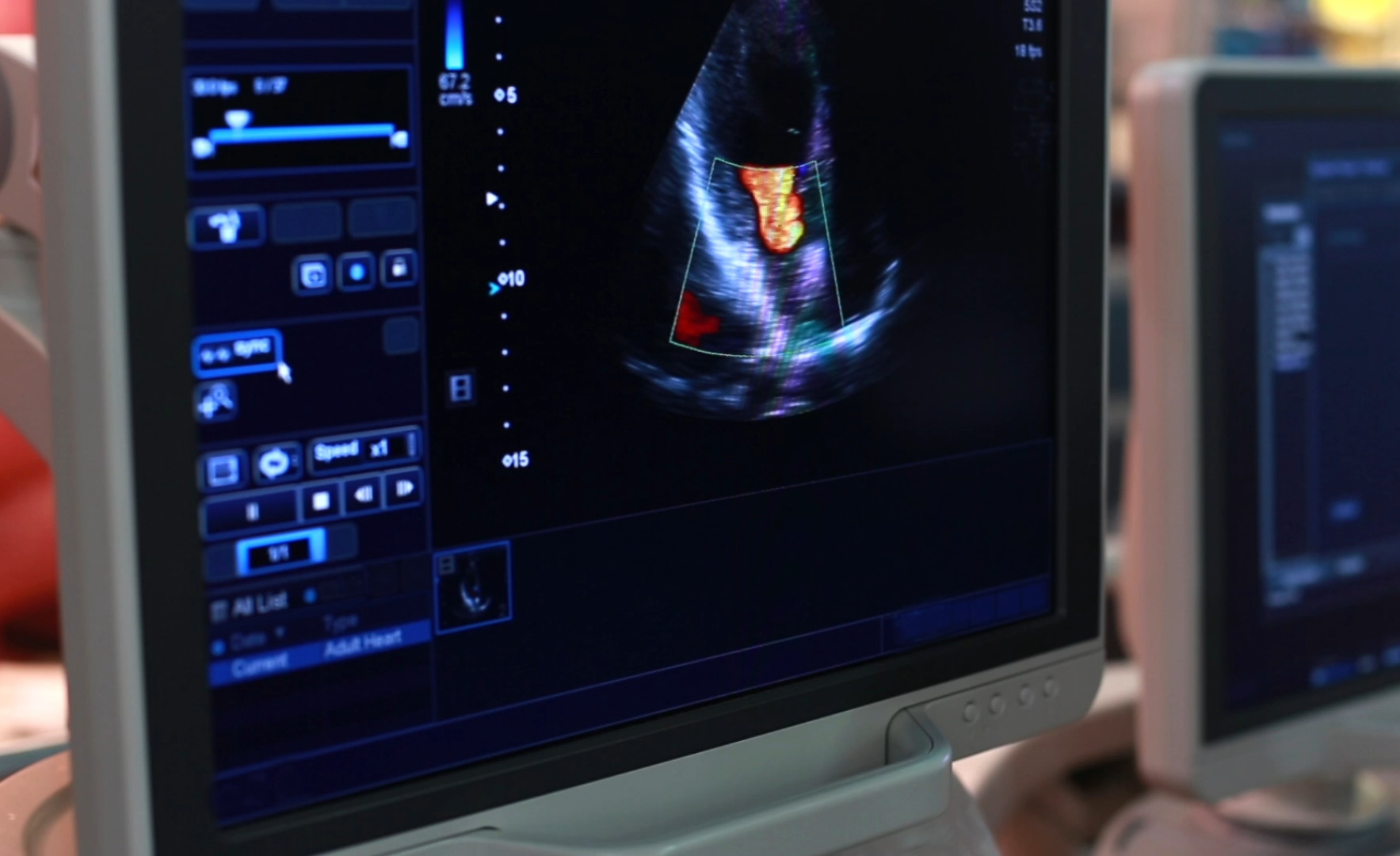
- Echocardiography is the best diagnostic tool to evaluate the severity of AR. A rough guideline for approximating severity is the width of the AR jet compared to the width of the left ventricular outflow tract:
- <1/3: Mild
- 1/3–2/3: Moderate
- >2/3: Severe
Management
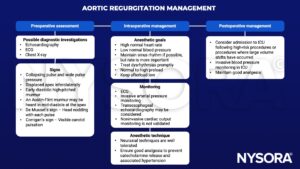
Acute severe AR management
- Sudden aortic incompetence results in acute pulmonary congestion
- Immediate management:
- Afterload reduction (nitroprusside)
- Enhancement of contractility and heart rate (dobutamine)
- Emergency surgical intervention is likely necessary
- Intra-aortic balloon pump is contraindicated
Suggested reading
- Flint N, Wunderlich NC, Shmueli H, Ben-Zekry S, Siegel RJ, Beigel R. Aortic Regurgitation. Curr Cardiol Rep. 2019;21(7):65.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Hines, R. L. (2017). Stoelting’s anesthesia and co-existing disease (7th ed.). Elsevier – Health Sciences Division
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2014 Jun 10;129(23):e650]. Circulation. 2014;129(23):2440-2492.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com