Learning objectives
- Describe the definition and underlying mechanisms of methemoglobinemia
- Diagnose methemoglobinemia
- Manage patients with methemoglobinemia
Background
- Methemoglobin is the form of the hemoglobin molecule where the iron moiety is oxidized (Fe3+)
- It is formed in the presence of an oxidizing substrate and does not carry oxygen
- It shifts the oxygen-hemoglobin dissociation curve to the left, hindering the unloading of oxygen to the tissues
- These effects are proportional to the concentration of methemoglobin and reversible
- Normal methemoglobin levels: 1-2 %
- Methemoglobinemia refers to an abnormally high concentration of methemoglobin and results in functional anemia
- Methemoglobinemia can be a life-threatening condition
Etiology
- Congenital (rare)
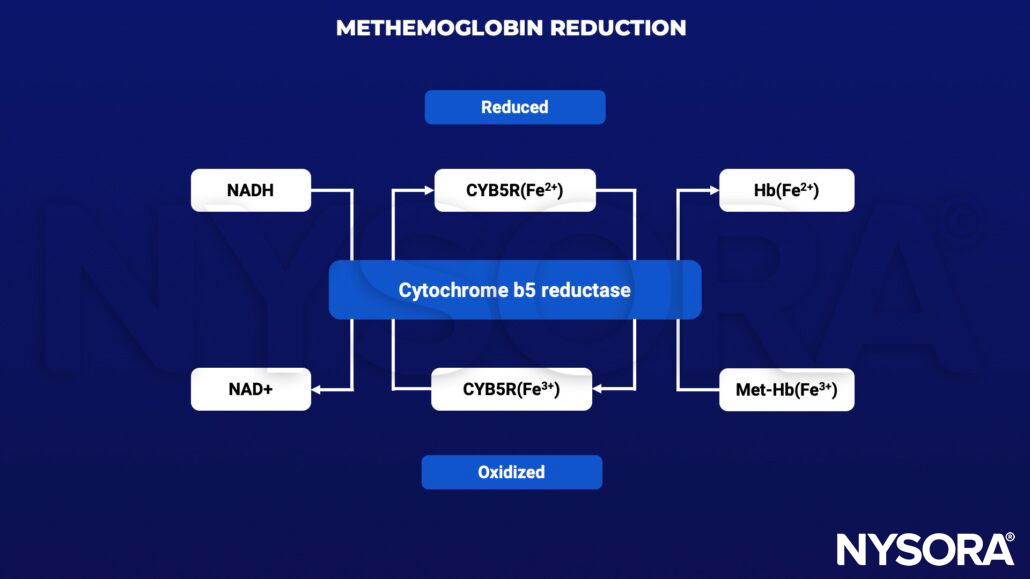
- Autosomal recessive defects in cytochrome b5 reductase (CYB5R)
- Congenital methemoglobinemia type I: CYB5R defect only in erythrocytes
- Congenital methemoglobinemia type II: CYB5R defect in all cells
- Autosomal dominant mutations in hemoglobins M (hemoglobin M disease)
- Autosomal recessive defects in cytochrome b5 reductase (CYB5R)
- Acquired
- Exposure to oxidizing agents leading to methemoglobin production that exceeds the body’s reduction capacity
- Oxidizing agents:
- Direct
- Benzocaine
- Prilocaine
- Lidocaine
- Tetracaine
- Indirect
- Nitrates, nitrites
- Metabolic activation
- Aniline
- Dapsone
- Direct
Pathophysiology
Reduction of methemoglobin by cytochrome b5 reductase:
- Hemoglobin M disease:
- Mutation in globin protein allows for stabilization of iron in the ferric state (Fe3+)
- Most patients have methemoglobin levels between 15-30% and remain asymptomatic
- Congenital methemoglobinemia: Defect in CYB5R function raising methemoglobin levels
- Acquired methemoglobinemia: CYB5R is overwhelmed by oxidative stress resulting in raised methemoglobin levels
Diagnosis
- Pulse oximetry measurements of oxygen saturation (SpO2): Refractory hypoxemia
- Refractory hypoxemia is usually not detected using blood gas analysis using the partial oxygen pressure (SaO2)
- Saturation gap: Difference between depressed SpO2 measurement and falsely normal SaO2 calculation
- A saturation gap >5% indicates the presence of abnormal forms of hemoglobin
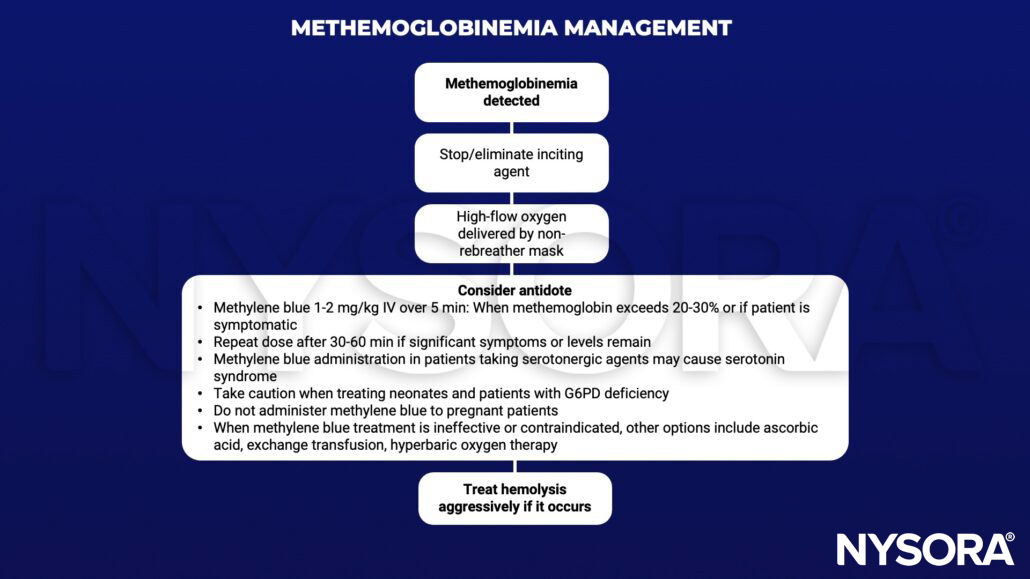
Management
Suggested reading
- Ludlow JT, Wilkerson RG, Nappe TM. Methemoglobinemia. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537317/
- Guay J. Methemoglobinemia related to local anesthetics: a summary of 242 episodes. Anesth Analg. 2009;108(3):837-845.
Clinical updates
Limper et al. (BJA, 2024) describe perioperative management of a patient with hereditary methemoglobinemia due to hemoglobin M (HbM Boston), highlighting that pulse oximetry and standard co-oximetry can be unreliable or misleading, even during profound physiological stress. The report emphasizes that methylene blue and ascorbic acid are ineffective in HbM variants, and instead supports management strategies focused on maintaining arterial oxygen content and global oxygen delivery (e.g., transfusion to increase CaO₂, monitoring lactate and DO₂ rather than SpO₂).
- Read more about this HERE.