Learning objectives
- Describe the mechanism and risk factors of laryngospasm
- Prevent laryngospasm
- Recognize and treat laryngospasm
Background
- Laryngospasm is the sustained closure of the vocal cords resulting in partial or complete loss of the airway
- Primitive protective airway reflex to prevent tracheobronchial aspiration after an offending stimulus
- Problematic prolongation of this initial reflex can occur under general anesthesia, often during intubation or extubation
- Can rapidly result in hypoxemia and bradycardia
- Overall incidence ~1%
- Incidence up to 25% in patients undergoing tonsillectomy and adenoidectomy
Signs
- Respiratory stridor
- Paradoxical respiratory movements
- Suprasternal and supraclavicular retractions
- Rapidly decreasing oxygen saturation
- Excessive chest movements but no movement of the reservoir bag and no capnogram reading
- Bradycardia
- Negative pressure pulmonary edema
- Cardiac arrest
- Pulmonary aspiration
- Arrhythmias
Risk factors
| Patient-related | Surgery-related | Anesthesia-related |
|---|---|---|
| Obesity | Nasal, oral or pharyngeal surgeries (adenoidectomy and tonsillectomy) | Laryngeal mask/Guedel airway device |
| Young age | Gastrointestinal endoscopy | Extubation |
| Active and passive smoking | Bronchoscopy | Suction catheter |
| ASA IV | Appendectomy | Light anesthesia plan |
| Gastroesophageal reflux | Anal or cervical dilatation | Blood/secretions in the airway |
| Obstructive sleep apnea | Mediastinoscopy | Regurgitation |
| Upper airway infection | Inferior urologic surgery | Desflurane |
| Hypocalcemia | Skin transplant | Ketamine and thiopental induction |
| Asthma | Nociception | Nasogastric tube |
| Difficult airway | Surgical stimulus | Inexperience of anesthesiologist |
| Movement | Failed intubation | |
| Recurrent laryngeal nerve damage | Laryngoscopy | |
| Esophageal stimulation | ||
| Iatrogrnic removal of parathyroid glands |
Prevention
- Anesthetic technique
- Ensure adequate depth
- Inhalation induction with non-irritant agent (e.g., sevoflurane)
- IV induction with propofol is less problematic
- Extubate either in a deep plane of anesthesia or fully awake, but not in-between
- “Deep” extubation: Suction the airway and place the patient in a lateral position
- Awake extubation: Once facial grimacing, adequate tidal volume, a regular respiratory pattern, coughing, and preferably eye opening have returned, use “no touch” technique: Pharyngeal suctioning and lateral positioning while anesthetized, followed by avoidance of any stimulation until eye opening when extubation is performed
- Extubation during forced positive pressure inflation decreases laryngeal adductor excitability, decreasing the risk of laryngospasm
- Pharmacological prevention
- Magnesium 15 mg/kg IV intraoperatively
- Lidocaine topically 4 mg/kg or IV 1.5-2 mg/kg (further research needed)
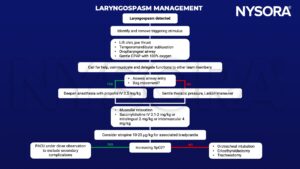
Management
Suggested reading
- Gavel G, Walker RWM. Laryngospasm in anaesthesia. Continuing Education in Anaesthesia Critical Care & Pain. 2014;14(2):47-51.
- Silva CR, Pereira T, Henriques D, Lanca F. Comprehensive review of laryngospasm. WFSA Resource Library. https://resources.wfsahq.org/uia/volume-35/comprehensive-review-of-laryngospasm/. Published July 8, 2020. Accessed February 2, 2023.
- Visvanathan T, Kluger MT, Webb RK, Westhorpe RN. Crisis management during anaesthesia: laryngospasm. Qual Saf Health Care. 2005;14(3):e3.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







