Learning objectives
- Pathophysiology of compartment syndrome
- Management of compartment syndrome
Definition and mechanism
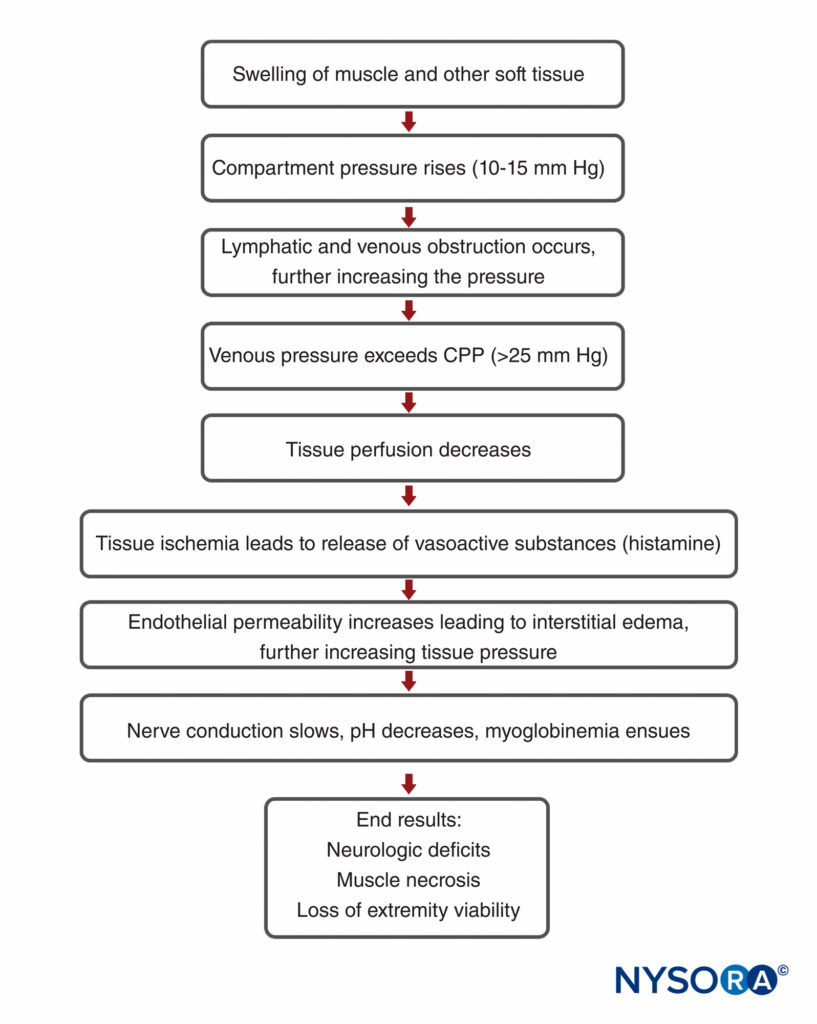
- Compartment syndrome is an orthopedic emergency and occurs when the pressure within a compartment increases
- Is essentially soft tissue ischemia, generally associated with trauma, fracture with subsequent casting, prolonged malpositioning during surgery, or reperfusion injury
- Because various osseofascial compartments have a relatively fixed volume, excess fluid or external constriction increases pressure within the compartment and decreases tissue perfusion
- The tissue hypoperfusion results in tissue hypoxia impeding cellular metabolism
- If prolonged, permanent myoneural tissue damage occurs
- As tissue pressure increases, extrinsic venous luminal pressure is exceeded, resulting in vein collapse
- Normal compartment pressure should be within 12-18 mmHg, a pressure above 18 mmHg is considered abnormal
- It is generally agreed that compartmental pressures greater than 30 mmHg require emergent intervention because ischemia is imminent
- Hypoxic injury causes cells to release free radicals, which increases endothelial permeability, leading to a vicious cycle of continued fluid loss, further increasing tissue pressure and injury
Signs and symptoms
| Acute compartment syndrome | Chronic compartment syndrome | |
|---|---|---|
| Characteristics | Occurs gradually, usually during and immediately after repetitive exercise Usually passes within minutes of stopping the activity Happens suddenly, usually after a fracture or severe injury A medical emergency that required urgent treatment Can lead to permanent muscle damage if not treated quickly | Occurs gradually, usually during and immediately after repetitive exercise Usually passes within minutes of stopping the activity Is not a medical emergency and does not cause permanent damage |
| Signs and symptoms | Intense pain, especially when the muscle is stretched, which seems much worse than would normally be expected for the injury Tenderness in the affected area Tightness in the muscle Paresthesia Numbness or weakness | Cramping pain during exercise, most often in the legs Swelling or a visibly bulging muscle A tingling sensation The affected area turning pale and cold In severe cases, difficulty moving the affected body part |
Etiology of acute compartment syndrome
| Conditions that increase the compartment volume | Conditions that lead to a reduction in the volume of tissue compartments |
|---|---|
| Direct soft tissue trauma with or without a long bone fracture Closed tibial shaft fractures and closed forearm fractures Soft tissue crush injuries Open fractures, which should theoretically decompress the adjacent compartments Hemorrhage: vascular injury, coagulopathy Anticoagulation therapy Revascularization of a limb after ischemia High-energy trauma, such as from high-speed motor vehicle accident or crush injury Increased capillary permeability after burns Infusions or high-pressure injections Extravasations of arthroscopic fluid Reperfusion after prolonged periods of ischemia Anabolic steroid use Decreased serum osmolarity (eg, nephritic syndrome) Strenuous exercise, especially in previously sedentary people | Tight circumferential dressings Closure of fascial defects Cast or splint, especially if placed before removal of the surgical tourniquet Prolonged limb compression, as in Trendelenburg and lateral decubitus positions Excessive traction to fractured limbs |
Complications of acute compartment syndrome
- Tissue necrosis
- Volkmann’s contractures
- Neurological deficits
- Gangrene
- Chronic regional pain syndrome
- Rhabdomyolysis with subsequent acute kidney injury
Diagnosis
- Based on clinical signs and symptoms
- Pain out of proportion to the injury, especially with passive stretch of the muscles in the suspicious compartment or limb
- A palpable tense extremity compared with the uninjured limb
- Paresthesia – late clinical sign
- Paresis – even later clinical sign
- Measure compartment pressure
- Maintain adequate pain control with the lowest possible dose in an attempt to avoid a delayed diagnosis of compartment syndrome
Management
Regional anesthesia and compartment syndrome
- Be cautious with regional anesthesia, as it may obscure signs and symptoms of acute compartment syndrome
- Avoid neuroaxial or periperhal regional techniques that result indense blocks of long duration
- Single-shot or continuous peripheral nerve blocks using lower concentrations of local anesthetic agents without adjuncts are considered safe as they are not associated with delays in diagnosis
Suggested reading
- Nathanson, M.H., Harrop‐Griffiths, W., Aldington, D.J., Forward, D., Mannion, S., Kinnear‐Mellor, R.G.M., Miller, K.L., Ratnayake, B., Wiles, M.D., Wolmarans, M.R., 2021. Regional analgesia for lower leg trauma and the risk of acute compartment syndrome. Anaesthesia 76, 1518–1525.
- Farrow C, Bodenham A, Troxler M. 2011. Acute limb compartment syndromes. Continuing Education in Anaesthesia Critical Care & Pain. 11;1:24-28.
- https://www.nysora.com/topics/sub-specialties/acute-compartment-syndrome-limb-implications-regional-anesthesia/
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







