Learning objectives
- Anesthetic management of lung cancer
Definition and mechanisms
- Lung cancer is the most common cause of cancer mortality worldwide for men and women
- Lung cancer or lung carcinoma is a malignant tumor characterized by uncontrolled cell growth in lung tissue
- Lung carcinomas derive from transformed, malignant cells that originate as epithelial cells, or from tissues composed of epithelial cells
- Sarcomas are generated by the malignant transformation of connective tissues, which arise from mesenchymal cells
- Lung cancer often starts in the bronchi, bronchioles, or alveoli
- Two types:
- Non-small-cell lung cancer
- The most common form, accounting for around 80% of lung cancer cases
- Common types include: squamous cell carcinoma, adenocarcinoma, or large-cell carcinoma
- Small-cell lung cancer
- Less common
- Spreads faster and harder to treat than non-small-cell lung cancer
- Non-small-cell lung cancer
- Other tumors including large cell, neuroendocrine (carcinoid), bronchioloalveolar and rarer forms can all present as lung malignancies
- The presentation includes airway obstruction, lung collapse, and distal infection or through spread via the peribronchial tissues with subsequent invasion of the mediastinum
- Spreads by both lymphatic and hematological routes and distal metastasis is common in the liver, adrenals, bone, and brain
Signs and symptoms
- A persistent cough
- Shortness of breath
- Chest pain
- Wheezing
- Hemoptysis
- Fatigue
- Hoarseness
- Weight loss
- Bone pain
- Headache
- Swelling in the face, neck, arms, or upper chest (superior vena cava syndrome)
Risk factors
- Smoking
- Older age
- Genetic mutations
- Exposure to harmful substances such as air pollution, radon, asbestos, uranium, silica, coal products
- Previous radiation treatment to the thorax
- Family history of lung cancer
Diagnosis
- Physical exam
- Blood test
- Chest X-ray
- CT/PET
- Biopsy
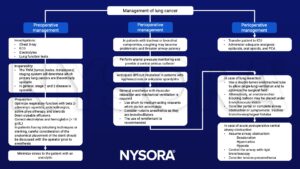
Management
- Anesthetic involvement is mainly for lung resection (e.g. lobectomy, pneumonectomy)
- Consider:
- Potentially compromised respiratory function with risk of perioperative respiratory complications
- Mass effects: obstructive pneumonia, lung abscess, SVC syndrome, tracheobronchial distortion, Pancoast’s syndrome, recurrent laryngeal nerve or phrenic nerve paresis, chest wall or mediastinal extension
- Metabolic effects: Lambert–Eaton syndrome, hypercalcemia, hyponatremia, Cushing’s syndrome
- Metastases: particularly to the brain, bone, liver, & adrenal
- Medications: chemotherapy agents, pulmonary toxicity (bleomycin, mitomycin), cardiac toxicity (doxorubicin), renal toxicity (cisplatin)
- Comorbidities including smoking, chronic obstructive lung disease, coronary artery disease, hypertension
Suggested reading
- Hackett, S., Jones, R., Kapila, R., 2019. Anaesthesia for pneumonectomy. BJA Education 19, 297–304.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com


