Learning objectives
- Define the signs and symptoms of multiple gestation pregnancies
- Describe the complications associated with multiple gestation pregnancies
- Management of multiple gestation pregnancies
Definition and mechanisms
- Multiple gestation is pregnancy with more than one fetus at a time, occurring in approximately 3% of all pregnancies
- Examples include pregnancy with twins, triplets, and quadruplets
- High-risk pregnancy requiring extra care
- Most women have multiple births via caesarean section
- Babies are often born prematurely and with a low birth weight → need to spend some time in the NICU
- The goal is to complete 37 weeks in twin pregnancies (considered term) → increases the chance that both babies will be born healthy and at a good weight
Signs and symptoms
- Exaggerated signs of pregnancy (e.g., extreme nausea and fatigue, severe vomiting)
- Faster than usual weight gain in the first semester of pregnancy
- Sore or very tender breasts
- Higher than normal levels of pregnancy hormones (i.e., human chorionic gonadotrophin)
- Higher than normal levels of protein alpha-fetoprotein in the mother’s blood
- Larger than usual belly compared to most women at a similar stage of pregnancy
- More than one fetal heartbeat
Causes
- One fertilized egg (ovum) splits before it implants in the uterine lining → monozygotic or identical twins
- Two (or more) separate eggs are fertilized by different sperm at the same time → dizygotic or fraternal twins
- Fraternal twins are more common than identical twins
- In a pregnancy with triplets or more, the babies could all be identical, all fraternal, or a mixture of both
Complications
Maternal
- Anemia
- Increased aortocaval compression
- Rapid desaturation
- Preterm prelabor rupture of membranes
- Preterm labor
- Prolonged labor
- Gestational hypertension
- Pre-eclampsia/eclampsia
- Gestational diabetes
- Placental abruption
- Disseminated intravascular coagulation
- Operative delivery
- Uterine atony
- Antepartum and postpartum hemorrhage
Fetal
- Preterm delivery
- Low birth weight
- Congenital anomalies (e.g., cerebral palsy)
- Polyhydramnios
- Cord entanglement
- Umbilical cord prolapse
- Fetal growth restriction, intrauterine growth restriction (IUGR), or small for gestational age
- Malpresentation (e.g., breech presentation)
- Increased mortality (i.e., miscarriage, stillbirth)
- Monochorionic twins (one placenta) risks that are unique to them
- Twin-twin transfusion syndrome
- Twin anemia polycythemia sequence
- Selective IUGR
Risk factors
- Family history of twins, triplets, or more increases the chance of multiple gestation pregnancy
- Fertility treatments
- Age ≥35 years (women are more likely to release more than one egg per cycle)
Management
All obstetric patients are considered to have a full stomach and be at risk for pulmonary aspiration, regardless of the time of last oral intake
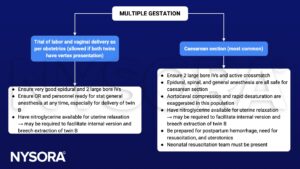
See also caesarean section considerations
See also premature infant considerations
See also postpartum hemorrhage considerations
Suggested reading
- Frölich M.A. (2022). Obstetric anesthesia. Butterworth IV J.F., & Mackey D.C., & Wasnick J.D.(Eds.), Morgan & Mikhail’s Clinical Anesthesiology, 7e. McGraw Hill. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=3194§ionid=266522956
- Rédai I (2013). Chapter 196. twin pregnancy, breech presentation, trial of labor after cesarean birth: anesthetic considerations for patients attempting vaginal birth. Atchabahian A, & Gupta R(Eds.), The Anesthesia Guide. McGraw Hill. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=572§ionid=42543788
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com

