Learning objectives
- Define and classify the different types of thyroidectomy
- Describe the complications that are associated with thyroidectomy
- Management of a patient undergoing a thyroidectomy
Definition and classification
- Thyroidectomy is the surgical removal of all or part of the thyroid gland
- The surgery is performed to treat thyroid disorders including thyroid cancer, a noncancerous enlargement of the thyroid (goiter), and overactive thyroid (hyperthyroidism)
- A skin crease incision is made approximately 4 cm above the sternum
- The recurrent laryngeal nerves and parathyroid glands should be preserved
Classification
- Total thyroidectomy: The entire thyroid gland is removed
- Near-total thyroidectomy: Both lobes of the thyroid are removed except for a small amount of thyroid tissue (on one or both sides) in the vicinity of the recurrent laryngeal nerve entry point and the superior parathyroid gland
- Partial thyroidectomies
- Hemithyroidectomy or unilateral thyroid lobectomy: One lobe of the thyroid is removed
- Isthmusectomy: The band of tissue (thyroid isthmus) connecting the two lobes of the thyroid is removed
- Open thyroid biopsy: The thyroid nodule is removed directly (rarely performed)
Indications
Thyrotoxicosis
- 2% of females, 0.02% of males
- Graves disease (hyperthyroidism) in younger women is the most common cause (up to 80%)
- Multinodular goiter (older patients)
- Toxic solitary nodule
- Other causes: Thyroiditis, pregnancy, drug-induced (amiodarone)
Thyroid malignancy
- Papillary (80%)
- 30-40 years old
- 95% 10-year survival rate
- Follicular (10%)
- May be hormone producing
- Older population
- 85% 10-year survival rate
- Medullary (8%)
- Older patients
- May be associated with multiple endocrine neoplasias
- May produce calcitonin
- 65% 10-year survival rate
- Anaplastic (1%)
- Mean survival 6 months from diagnosis
Patient characteristics
- Up to 5% of the population has a goiter
- Most patients are female
- Approximately 10% of thyroid nodules will be malignant
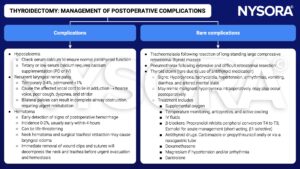
Complications
- Hypothyroidism → need for lifelong thyroid hormone replacement
- Recurrent laryngeal nerve palsy
- Unilateral damage: Temporary or permanent hoarseness
- Bilateral damage: Airway obstruction and acute respiratory distress
→ emergency tracheostomy may be required
- Damage to the parathyroid glands → temporary or permanent hypoparathyroidism and hypocalcemia
- Anesthetic complications
- Infection
- Hemorrhage/hematoma which may compress the airway → acute respiratory distress
- Stich granuloma
- Chyle leak
Management
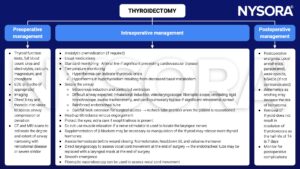
Preoperative assessment
Detailed history and examination
- Airway
- Marked tracheal deviation
- Stridor or respiratory distress, especially when supine
- Assess vocal cords movement to recognize preexisting laryngeal nerve palsy
- Cardiovascular system
- Hyperthyroidism can cause tachycardia, atrial fibrillation, or heart failure
- Large goiters may obstruct venous drainage, and superior vena cava obstruction can occur with retrosternal spread
- Eyes
- Protect the eyes from intraoperative drying or trauma in case of lid retraction and exophthalmos
- Other conditions
- May be part of multiple endocrine neoplasia syndromes, and conditions such as diabetes mellitus, hyperparathyroidism, and pheochromocytoma must be considered
Drug treatment in hyperthyroidism
Patients should be clinically and biochemically euthyroid before surgery
- Carbimazole: Inhibits iodination of tyrosyl residues in thyroglobulin
- Propylthiouracil: Same as carbimazole but also reduces peripheral deiodination of T4 to T3
- β-blockers: Control cardiovascular effects; propranolol also decreases the extrathyroidal conversion of T4 to T3
- Iodine: Give potassium iodine for 7-10 days preoperatively
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 20 Head and neck surgery, Macnab R and Bexon K.
We would love to hear from you. If you should detect any errors, email us [email protected]