Case Study: Cervical Hernia with Radicular Pain
Cervical disc herniation is a common condition that can cause significant pain, particularly when it leads to radicular pain. This article provides an in-depth look at a case of cervical hernia with radicular pain, detailing the diagnosis, treatment, and outcome. The focus will be on the Percutaneous Laser Disc Decompression (PLDD) procedure, a minimally invasive treatment option for patients with disc herniation who have not responded to conservative therapy.
Case presentation
A 41-year-old woman presented with cervical pain radiating to her left upper limb. The pain was aggravated by physical activities, including CrossFit, and was described as persistent, with shock-like sensations, pins and needles, and burning feelings.
- Pain intensity: Baseline pain was measured at 4/10 on the Numerical Rating Scale (NRS), peaking at 8/10 during episodes of exertion.
- Neurological evaluation: A detailed physical examination confirmed radicular pain following the C7 nerve root dermatome.
Diagnosis
Medical history and symptoms
The patient reported no prior medical conditions but engaged in frequent high-intensity exercises, which may have contributed to the worsening of symptoms. The pain was consistent with radiculopathy, a condition characterized by nerve irritation due to a herniated disc.
- Physical examination findings: The Spurling test, a diagnostic maneuver used to assess cervical nerve root compression, was positive. The test aggravated the patient’s neck pain and reproduced the arm pain, indicating C7 nerve root involvement.
- Imaging: Magnetic Resonance Imaging (MRI) revealed a C6-C7 posterior disc protrusion with mild left-sided uncovertebral arthrosis, moderately narrowing the neural foramen.
Final diagnosis
The patient was diagnosed with cervical radiculopathy, specifically brachial plexus root pain caused by the C6-C7 disc herniation. This type of pain results from compression or irritation of the cervical nerve roots, often leading to pain that radiates down the arm.
Treatment: Percutaneous Laser Disc Decompression (PLDD)
What is PLDD?
PLDD is a minimally invasive outpatient procedure performed under local anesthesia. It is designed to relieve pain from contained disc herniation by reducing the size of the protruding disc through laser application.
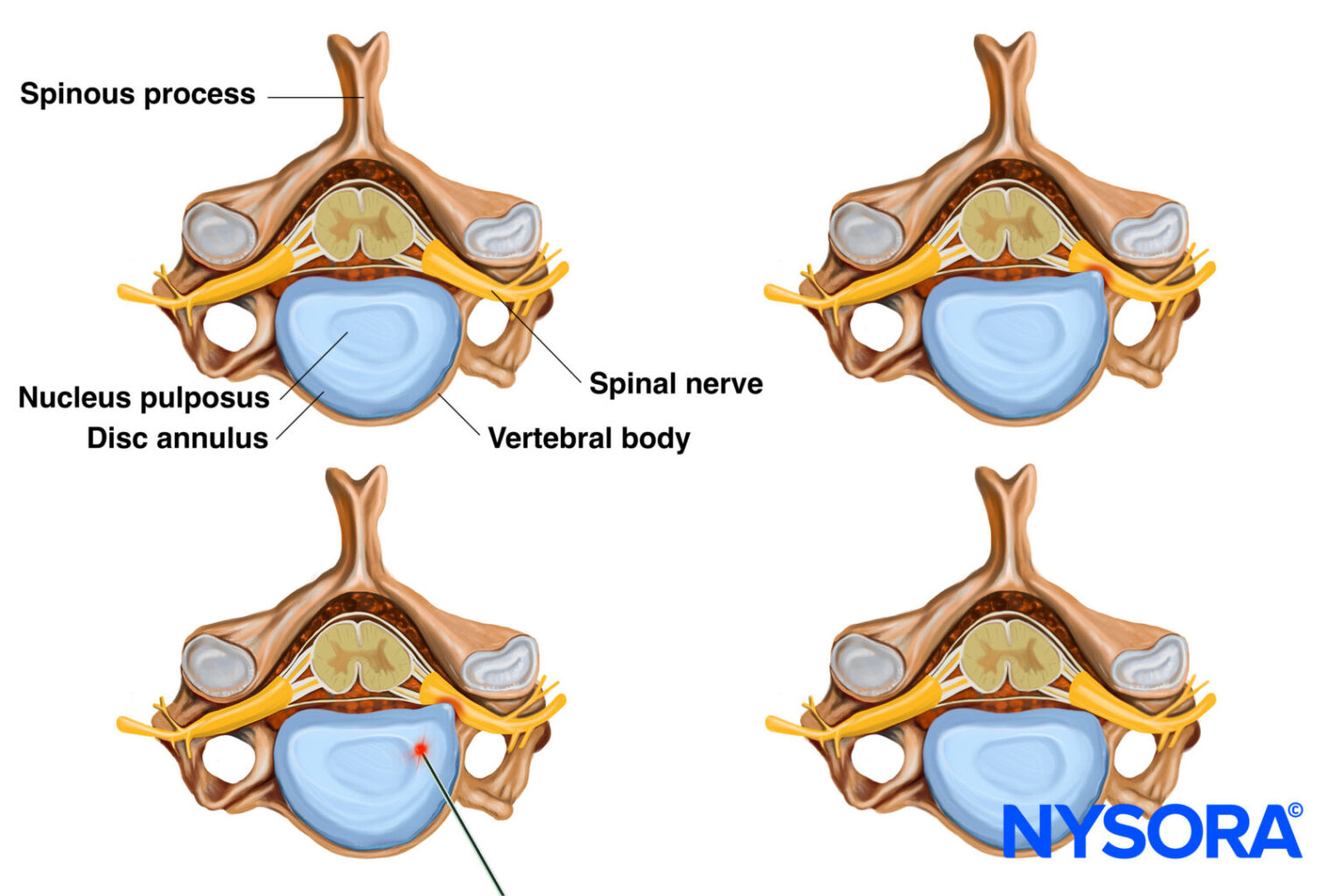
PLDD involves the percutaneous insertion of an optical fiber into the herniated disc, through which a laser is applied to reduce the disc’s herniation.
Indications for PLDD
PLDD is suitable for patients with contained cervical disc herniations, such as bulging or protrusion, which cause neck and/or radicular pain. It is often recommended for individuals who do not respond to conservative treatments like physical therapy or medication.
Step-by-Step PLDD Procedure
- Patient preparation:
- The patient is placed in a supine position with a head-ring pillow to support the neck. Conscious sedation may be administered using intravenous (IV) propofol for anxious patients.
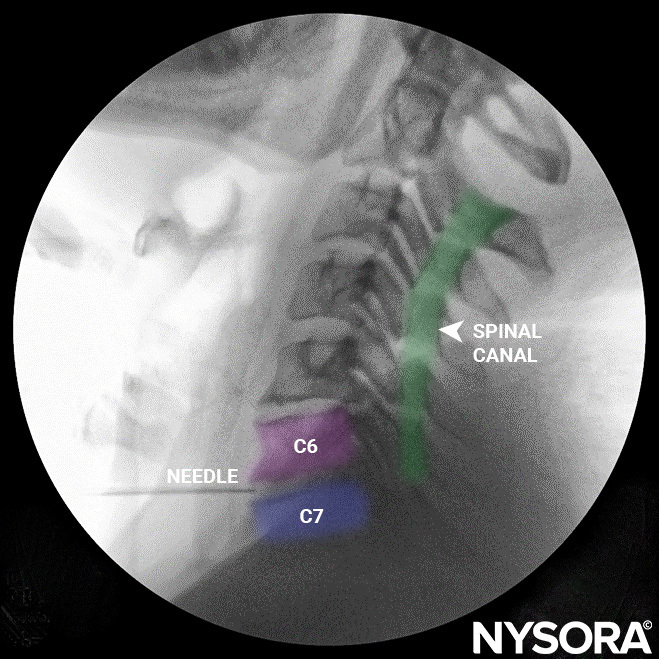
- The cervical spine is identified under fluoroscopic guidance.
- Needle insertion:
- A 22-gauge needle is inserted through the front of the neck, using a three-finger technique to avoid damage to the trachea, esophagus, and blood vessels.
- Fluoroscopy is used to guide the needle into the nucleus pulposus of the C6-C7 disc.
3. Laser application:
-
- Once the needle is in place, an optical fiber is passed through the needle, and a laser is applied to shrink the protruding disc. This relieves the pressure on the nerve root, alleviating radicular pain.
4. Tips for a safe and effective procedure:
-
- The procedure should always be performed under antibiotic prophylaxis to prevent infection.
- The laser fiber should not extend beyond the middle third of the disc to avoid potential spinal cord injury.
- Careful evaluation of the thyroid gland is necessary, particularly if thyroid cysts are present, to avoid accidental puncture.
Monitoring during the procedure
Patients undergoing PLDD are monitored closely:
- Vital signs: Electrocardiography (ECG), blood pressure, and oxygen saturation are continuously monitored.
- Anesthesia: Local infiltration with 2% lidocaine is used, and conscious sedation with propofol may be administered for comfort.
Patient outcome
Short-term follow-up
At the 4-week follow-up appointment:
- The patient reported no pain (NRS 0/10) during rest or light physical activities.
- Mild paresthesia (numbness or tingling) was still present in the C7 dermatome.
Long-term follow-up
At the 8-week follow-up:
- The patient remained pain-free (NRS 0/10), even during intense exercise.
- No residual paresthesia was reported, indicating full resolution of radicular symptoms.
Key benefits of PLDD
- Minimally invasive: The procedure is less invasive than traditional surgery, leading to faster recovery and fewer complications.
- Outpatient setting: PLDD can be performed as an outpatient procedure, reducing the need for hospital stays.
- High success rate: Many patients, including the one in this case, experience significant pain relief and improved quality of life following PLDD.
Conclusion
Cervical disc herniation with radicular pain can significantly affect a patient’s quality of life. In this case, a 41-year-old woman achieved complete pain relief following percutaneous laser disc decompression. This minimally invasive procedure offers a safe and effective alternative to traditional surgery, with the added benefits of a quicker recovery and fewer complications. As this case illustrates, PLDD is a promising option for patients with cervical disc herniation, providing long-term relief from radicular pain.
Interested in more details about this procedure? Download NYSORA’s Pain Rx App to discover more!