Assessing erector spinae plane blocks for improved recovery in adolescent spinal fusion surgery
Adolescent idiopathic scoliosis (AIS) is a condition affecting 1-3% of adolescents aged 10-16, characterized by a curvature of the spine with no identifiable cause. For most patients, this condition remains mild and manageable, but in severe cases, surgical intervention through posterior spinal fusion (PSF) becomes necessary. Effective pain management following PSF is crucial to ensuring a smooth recovery and enhancing patient outcomes. Currently, multimodal analgesia, which involves combining various pain relief methods, is the standard approach. However, the role of advanced regional anesthesia techniques, such as the erector spinae plane block (ESPB), remains under-explored in pediatric populations.
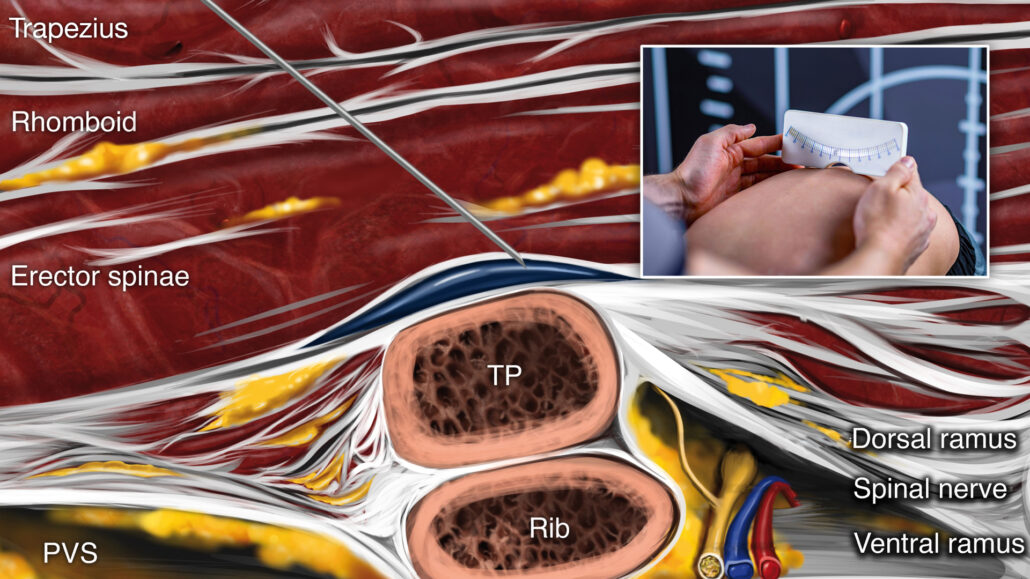
The ESPB is a novel regional anesthesia technique that involves injecting a local anesthetic near the spine to block pain transmission effectively. This technique has shown promising results in managing pain in adult spine surgeries and some pediatric procedures. However, its use in pediatric patients undergoing PSF for AIS has been limited. This study aimed to evaluate the practicality and effectiveness of integrating ESPB into a rapid recovery pathway for pediatric patients following PSF.
Study objective and methods
This prospective, randomized controlled trial enrolled 24 patients aged 10-19 years, all of whom were undergoing multilevel PSF for AIS correction. Patients were excluded if they had chronic pain conditions requiring neuromodulating medications, neuromuscular scoliosis, a history of chronic opioid therapy, or allergies/contraindications to the study medications or techniques.
Participants were randomly assigned to two groups: one group of 12 patients received bilateral ESPB before the surgical incision, while the other 12 patients served as the control group and did not receive ESPB. ESPBs were administered using ultrasound guidance to inject a mixture of 0.25% bupivacaine and dexamethasone near the T7 vertebrae. Patients were evaluated at multiple time points for pain scores, satisfaction, and opioid consumption (oral morphine equivalents) during their hospital stay.
The primary outcome was to assess the practicality of incorporating ESPB into a rapid recovery protocol for pediatric patients undergoing PSF for AIS correction. Secondary outcomes included comparing opioid consumption (measured as oral morphine equivalents, OME) and pain levels using the numerical rating scale (NRS) between patients receiving ESPB and those who did not.
Key findings
Primary outcome
ESPB was successfully integrated into the rapid recovery pathway for 11 out of 12 patients in the ESPB group. The procedure was aborted in 2 patients due to anatomical variations, highlighting some limitations in its universal applicability.
Secondary outcomes
- Opioid consumption: The total OME used by patients in the ESPB group (195.5) were not significantly different from those in the control group (138.0); p = 0.06.
- Pain scores: There were no statistically significant differences in NRS pain scores at rest or during movement between the two groups at various time points.
Additional observations
The study found that ESPB could be a practical addition to the pain management protocol, but anatomical variations in patients might limit its application. Furthermore, no significant differences in patient satisfaction or length of hospital stay were observed between the two groups.
Conclusion
This study demonstrated that the ESPB could be successfully integrated into a rapid recovery pathway for pediatric patients undergoing PSF for AIS. However, its impact on reducing opioid use and pain levels was not significantly different from standard pain management approaches. While the ESPB showed promise as a practical tool for managing postoperative pain, the findings suggest that its overall effectiveness may be influenced by individual anatomical differences and patient selection.
Future research
Further research could focus on refining patient selection criteria, exploring optimal timing for the block, and developing strategies to maximize the benefits of ESPB in multimodal pain management for spinal fusion surgeries.
For more detailed information, refer to the full article in RAPM.
Ruby J, Popovic M, Illescas A, et al. Multimodal analgesia and the erector spinae plane block in a rapid recovery pathway after posterior spinal fusion in adolescent idiopathic scoliosis: a randomized controlled study of practicality. Reg Anesth Pain Med. Published online September 16, 2024.
Download the Nerve Blocks App HERE for in-depth insights on the erector spinae plane block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks!