eFAST: A valuable tool in trauma diagnosis
The extended Focused Assessment with Sonography in Trauma (eFAST) is a valuable diagnostic tool for quickly assessing trauma patients. It helps identify life-threatening conditions such as pneumothorax, cardiac tamponade, and intra-abdominal free fluid, which are common after blunt or penetrating trauma. Using point-of-care ultrasound (POCUS), eFAST allows healthcare providers to make rapid decisions about patient care, especially in the emergency department.
What is eFAST?
The FAST (Focused Assessment with Sonography in Trauma) exam was one of the earliest applications of POCUS and primarily focused on detecting free fluid in the abdomen. The eFAST exam expands on this by including an evaluation of the lungs to detect pneumothorax or intrathoracic fluid, making it an essential tool for trauma cases. A positive eFAST exam in an unstable patient can prompt immediate surgical intervention to prevent further deterioration.
Key indications for eFAST:
- Pneumothorax: Collapsed lung that may cause breathing difficulties.
- Intrathoracic fluid: Accumulation of fluid in the chest cavity.
- Cardiac tamponade: Fluid accumulation around the heart leads to decreased cardiac output.
- Intra-abdominal free fluid: Blood or other fluid in the abdominal cavity, often indicating internal bleeding.
Essential information about eFAST
- eFAST should be performed as part of the “C” (Circulation and Hemorrhage Control) in the ABC approach to trauma.
- eFAST can be used for both blunt and penetrating trauma, though the sensitivity in penetrating trauma improves with repeated scanning.
- A positive eFAST exam can indicate significant internal bleeding or trauma, which may require immediate surgery.
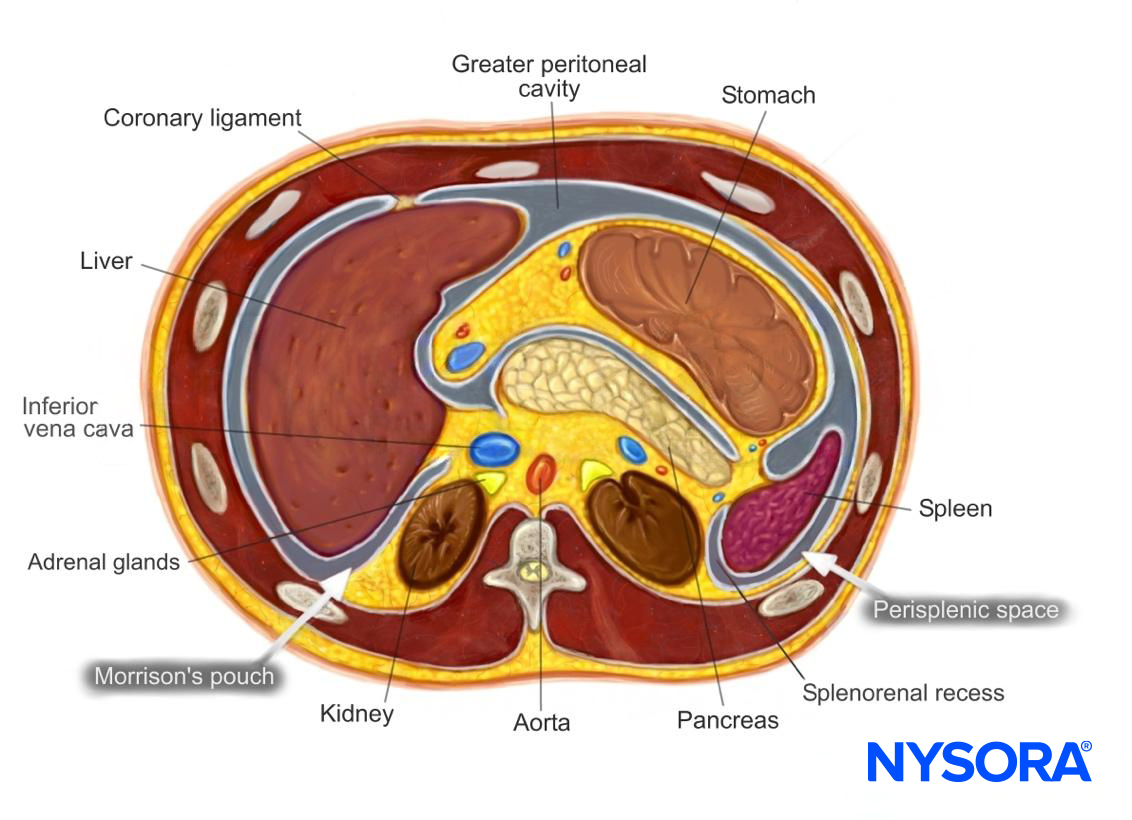
Anatomy & fluid collection sites
Intraperitoneal fluid tends to accumulate in specific anatomical locations due to gravity. These include:
- Morrison’s pouch: Between the liver and kidney.
- Perisplenic space: Around the spleen.
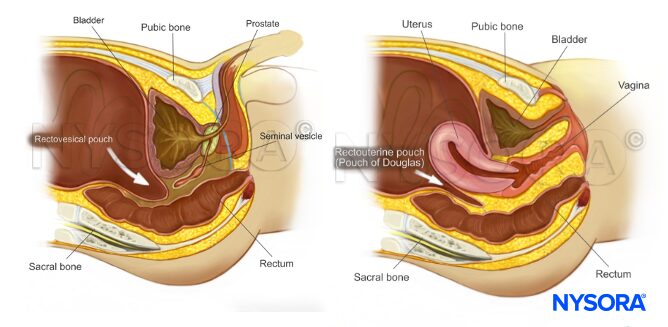
- Rectovesical pouch (in males) or rectouterine pouch (in females): Located in the pelvis, behind the bladder or uterus.
eFAST examination technique
Ultrasound machine setup:
- Transducer: Curvilinear or phased array.
- Depth: 8-20 cm (adjust based on target structures).
- Preset: Use the abdominal or FAST setting.
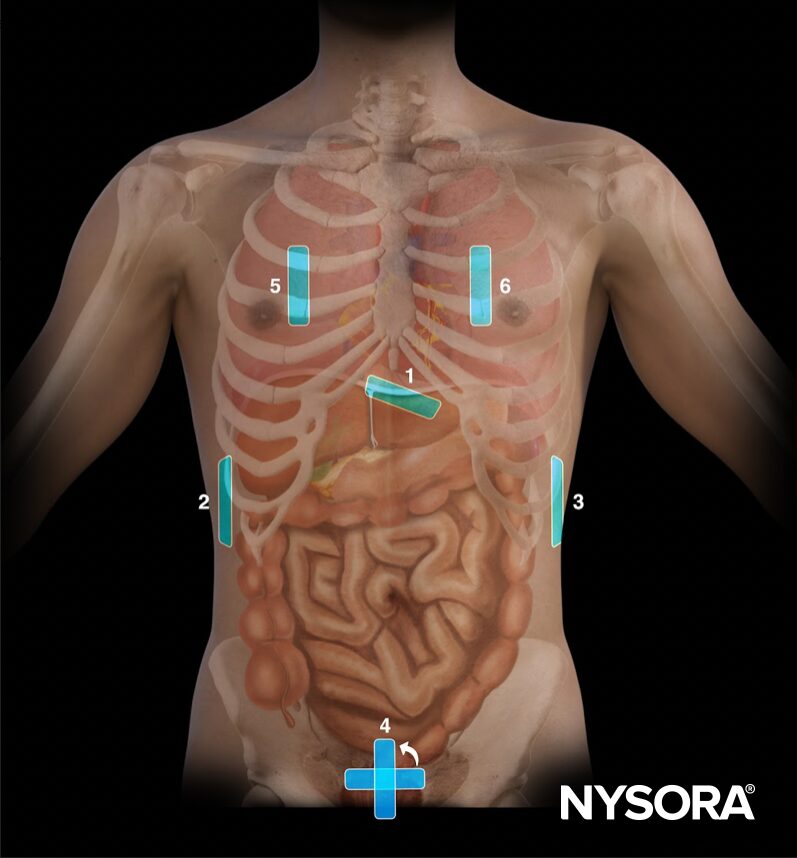
The patient is placed supine with arms abducted, and the transducer is applied in six key positions to examine different areas of the chest and abdomen.
- Subcostal view (cardiac assessment): Used to detect pericardial effusion or cardiac tamponade.
- Right upper quadrant (RUQ): Scans for fluid in Morrison’s pouch between the liver and kidney.
- Left upper quadrant (LUQ): Looks for free fluid in the perisplenic space or splenorenal recess.
- Pelvic view: Checks for fluid in the rectovesical pouch (males) or rectouterine pouch (females).
- Right lung: Scans for pneumothorax or fluid in the right thorax.
- Left lung: Scans for pneumothorax or fluid in the left thorax.
Key findings in eFAST
Tamponade detection:
- The subcostal view helps identify cardiac tamponade by showing an anechoic (black) fluid layer around the heart.
- In cases of cardiac arrest or deep shock, immediate intervention, such as pericardiocentesis, may be required.
Free intraperitoneal fluid:
- Fluid typically collects in areas like Morrison’s pouch and the perisplenic space. Free fluid on eFAST may indicate hemorrhage or injury to the liver, spleen, or other abdominal organs.
Pneumothorax detection:
- The absence of lung sliding during scanning suggests a pneumothorax. Other signs include the stratosphere sign on M-mode imaging.
Clinical impact of eFAST
In trauma cases, time is critical. The eFAST exam provides rapid, point-of-care diagnostic information that can drastically reduce the time to treatment, especially in unstable patients. With a clear eFAST protocol, healthcare providers can efficiently evaluate patients, rule out life-threatening conditions, and direct care toward the most urgent interventions.
Want to learn more about eFAST and other POCUS protocols? Download NYSORA’s POCUS App!