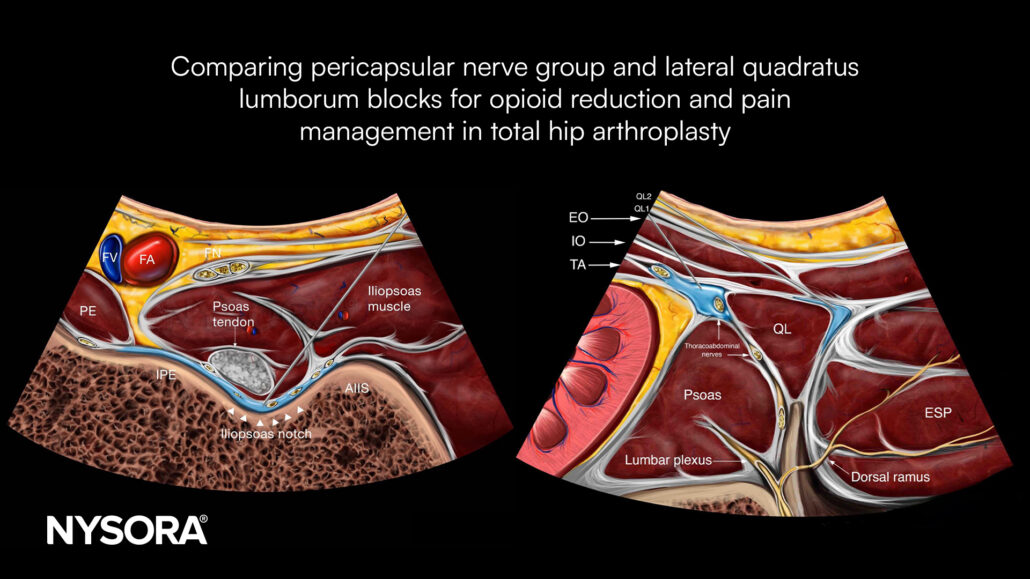
Comparing pericapsular nerve group and lateral quadratus lumborum blocks for opioid reduction and pain management in total hip arthroplasty
Total hip arthroplasty (THA) is a common orthopedic procedure, and effective postoperative pain management is crucial for enhancing recovery. Regional anesthesia techniques, such as the pericapsular nerve group (PENG) and lateral quadratus lumborum block (QLB), are designed to reduce opioid use while providing pain relief. This study compares the efficacy of these two techniques in managing postoperative pain and reducing opioid consumption after THA.
Study objective and methods
The primary objective of this randomized controlled trial was to assess whether the PENG block, when combined with a lateral femoral cutaneous nerve (LFCN) block, provided superior analgesia compared to the lateral QLB in patients undergoing elective THA. A total of 106 patients participated in this study, all of whom were randomly assigned to receive either the PENG + LFCN block or the lateral QLB.
- Primary outcome: The cumulative opioid consumption was measured over 72 hours post-surgery, using intravenous morphine milligram equivalents (MMEs) to standardize results. This allowed for a direct comparison of opioid use between the two groups.
- Secondary outcomes: Additional outcomes included postoperative pain scores during both movement and rest, time to ambulation, length of hospital stay, and functional outcomes. Functional outcomes were assessed using the Hip Disability and Osteoarthritis Outcome Score (HOOS JR) and the Patient-Reported Outcome Measures Information System (PROMIS-10).
Key findings
- Opioid consumption: At 72 hours post-surgery, patients in the QLB group consumed significantly fewer opioids than the PENG + LFCN group (mean difference of 33 mg, p = 0.001). Statistically significant differences in opioid consumption were also observed at 36 hours (mean difference of 18 mg, p = 0.040), 48 hours (23 mg, p = 0.011), and 60 hours (28 mg, p = 0.004).
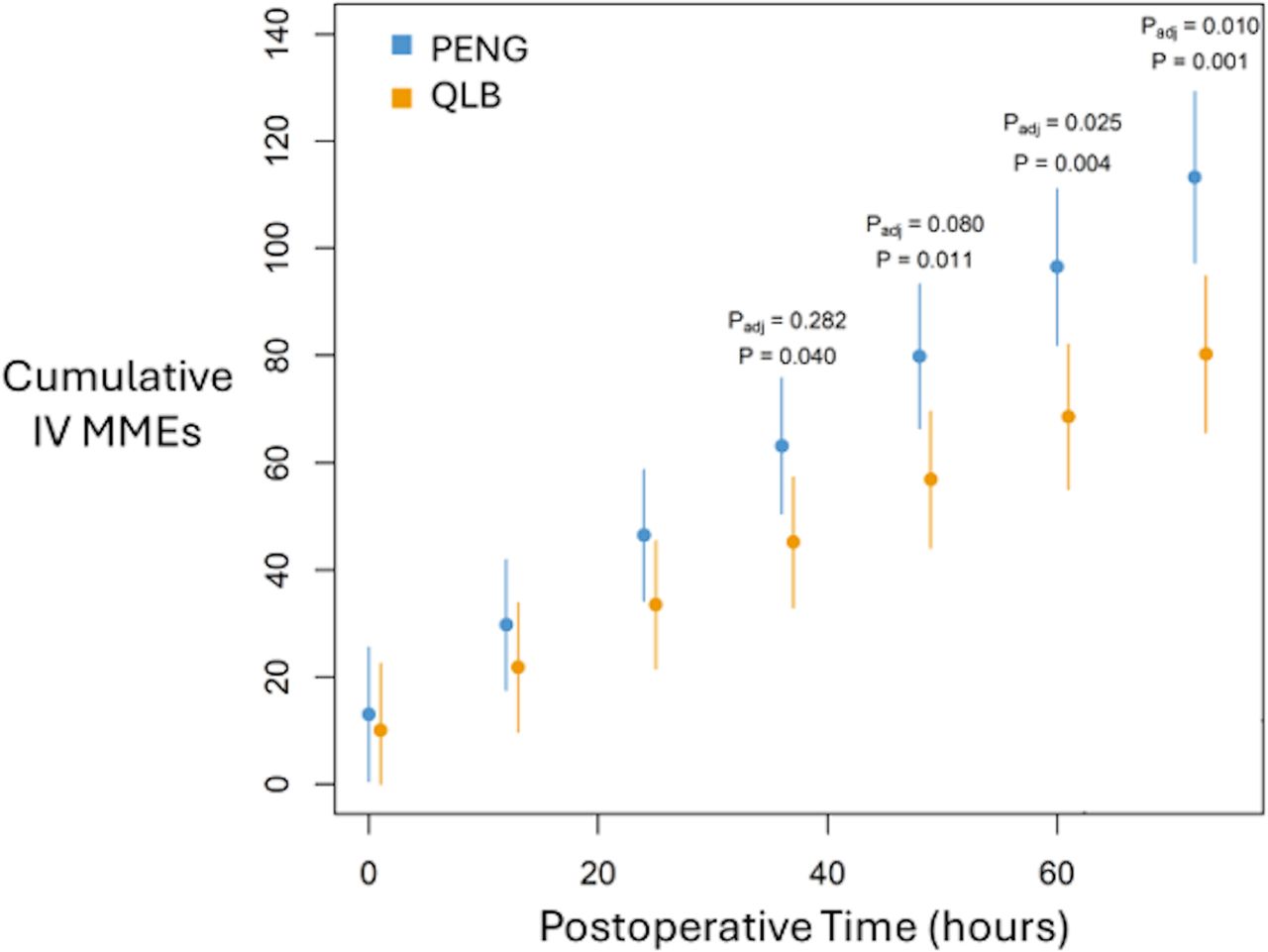
Cumulative opioid consumption. IV MME, intravenous morphine milligram equivalents; PENG, pericapsular nerve group; QLB, quadratus lumborum block. P-values are from linear contrasts for a linear mixed model including block, time, and the block x time interactions. P: not adjusted for multiple comparisons. Padj: Bonferroni corrected for pairwise comparisons.
- Pain with movement: The lateral QLB group reported lower pain scores during movement from 36 to 72 hours postoperatively.
- Resting pain scores: Both groups experienced similar levels of pain relief at rest.
- Functional outcomes: There were no significant differences between groups in terms of time to ambulation, length of hospital stay, or functional outcomes (HOOS JR and PROMIS-10 scores).
Conclusion
The study concluded that the lateral QLB is superior to the PENG + LFCN block in terms of reducing postoperative opioid consumption and managing pain during movement in the early recovery period following THA. Both blocks effectively managed pain at rest and supported early ambulation, but the opioid-sparing benefits and improved movement-related pain control make the QLB a potentially preferable choice for post-THA pain management.
The QLB’s ability to target the thoracolumbar fascia and abdominal musculature may contribute to its wider analgesic effect, which could explain its efficacy in controlling pain during movement. This block not only addresses the need for lower opioid use but also aligns with current pain management goals in THA by supporting rapid recovery and minimizing dependency risks.
Future research
Further research is encouraged to refine these techniques and determine optimal local anesthetic volumes, particularly for the QLB. Future studies might focus on examining the effectiveness of these blocks in various surgical approaches to THA, such as anterior, lateral, and posterior approaches, to assess whether one technique might offer distinct advantages depending on the surgical approach. Long-term studies on patient outcomes and functional recovery metrics would also be beneficial in assessing the broader impact of these anesthesia techniques beyond the immediate postoperative period.
For more detailed information, refer to the full article in RAPM.
Hay E, Kelly T, Wolf BJ, et al. Comparison of pericapsular nerve group and lateral quadratus lumborum blocks on cumulative opioid consumption after primary total hip arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. Published online October 10, 2024.
Download the Nerve Blocks App HERE for in-depth insights on the supraclavicular brachial plexus block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks!




