A novel point-of-care ultrasound method for assessing diaphragmatic excursion
A recent study published in Regional Anesthesia and Pain Medicine (2024) introduces a novel approach to evaluating diaphragmatic function using point-of-care ultrasound (POCUS). Conducted by Dr. Diogo Da Conceicao and colleagues at Toronto Western Hospital, this research compares a novel method against two established techniques, highlighting its potential for enhanced diagnostic accuracy.
Background
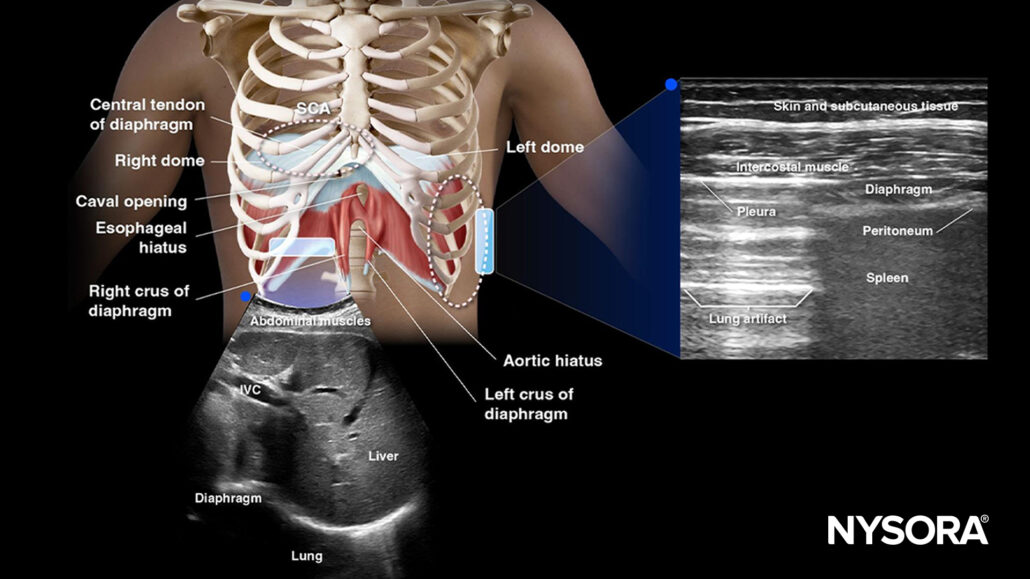
The diaphragm, a crucial muscle for respiration, is often affected during certain medical procedures like brachial plexus blocks or surgeries involving the thoracic cavity. Traditional methods to evaluate diaphragmatic motion include:
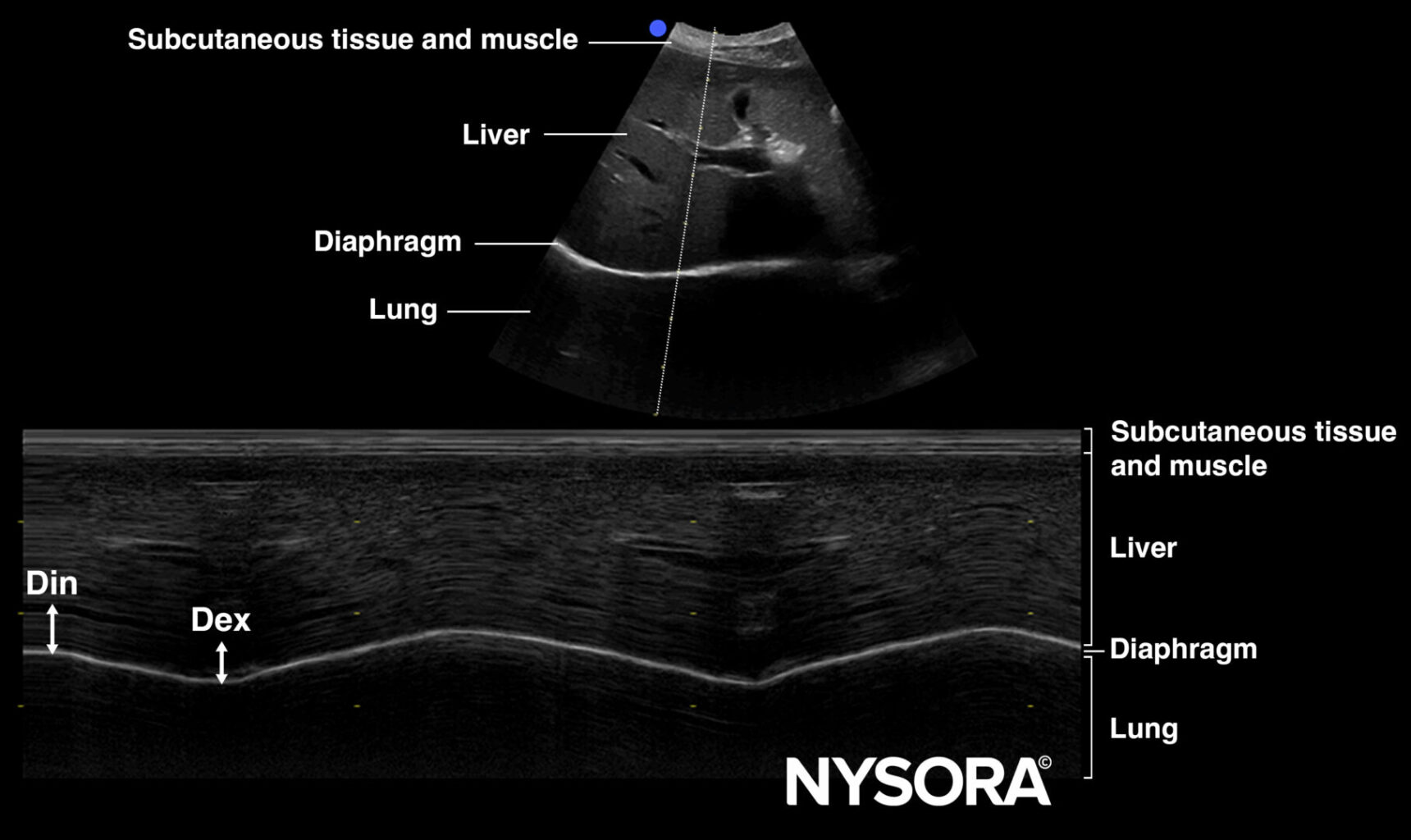
- Excursion of the Dome of the Diaphragm (DOD): Uses a curvilinear transducer to measure motion through the abdomen by scanning the subcostal area.
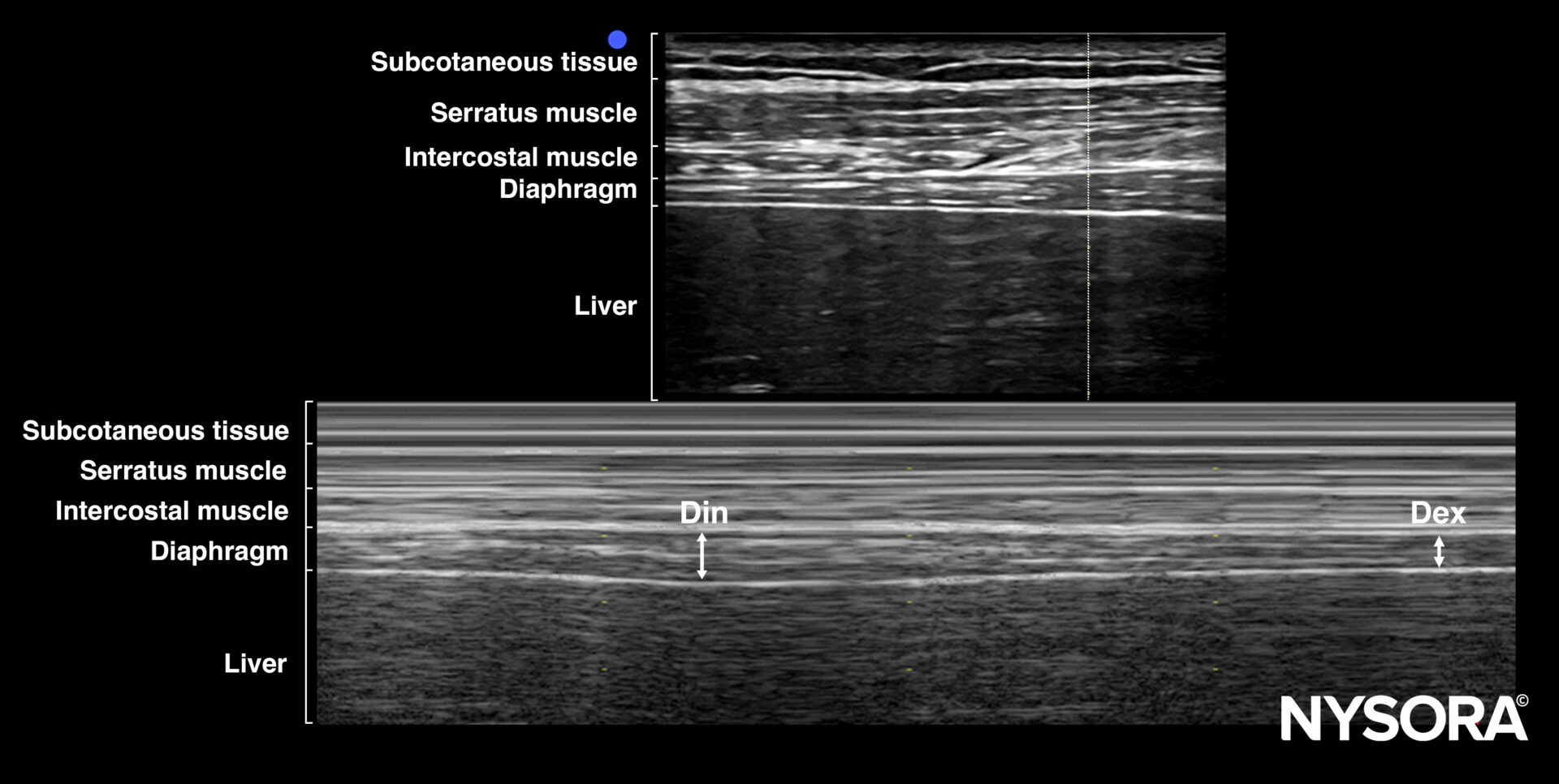
- Thickening fraction of the Zone of Apposition (ZOA): Examines diaphragmatic thickening during inspiration with a linear probe.
However, these methods face limitations:
- Left-side DOD measurements are challenging due to a narrow acoustic window.
- ZOA thickening measurements can be inconsistent due to variability in readings.
To address these issues, the study explores measuring ZOA excursion via a high-frequency linear transducer placed at the mid-axillary line.
Study design
Participants:
- 75 elective surgical patients with normal diaphragmatic function.
- Exclusion criteria: abnormal pulmonary function, pre-existing diaphragm dysfunction, or BMI > 35 kg/m².
Methods:
- Three ultrasound techniques were assessed:
- DOD excursion: Measured using a 2–5 MHz curved transducer.
- ZOA thickening fraction: Examined via a linear transducer in the lateral chest.
- ZOA excursion: Distance between end-inspiration and end-expiration of the ZOA’s uppermost point.
Primary outcome: Success rate in capturing clear ultrasound views.
Secondary outcomes: Procedure time and correlation among methods.
Key findings
- High success rate for ZOA excursion:
- 100% success for both left and right sides compared to 98.7% (right) and 34.7% (left) for DOD excursion.
- ZOA excursion is unaffected by the narrow acoustic window that hampers DOD assessments.
- Procedure times:
- Median times for ZOA and DOD excursion measurements ranged between 1.9 and 5.1 minutes.
- Minimal differences in time efficiency between the methods.
- Correlation between methods:
- ZOA excursion values showed strong agreement with DOD excursion values, particularly on the right side.
- Challenges with ZOA thickening fraction:
- High variability and lack of significant correlation with other methods.
Clinical implications
The novel ZOA excursion method offers several advantages:
- Reliability: Consistently successful in capturing diaphragmatic motion, even on the left side.
- Ease of use: Requires less expertise than the DOD method.
- Applicability: Useful for diagnosing conditions like diaphragmatic paresis, especially in perioperative settings.
Future research will be essential to:
- Define normal reference values.
- Establish diagnostic thresholds for diaphragmatic dysfunction.
- Evaluate its application in diverse patient populations, including those with obesity or respiratory compromise.
Step-by-step guide: Performing ZOA excursion assessment
- Position the patient: Semi-recumbent position.
- Place the transducer: Use a linear 10–12 MHz transducer along the mid-axillary line.
- Identify the ZOA: Locate the most cephalad point of contact during inspiration and expiration.
- Measure excursion: Record the distance between these two points.
Conclusion
This study highlights the potential of ZOA excursion measurement as a reliable alternative for assessing diaphragmatic motion. With further validation, it could become a standard tool in clinical settings, aiding anesthesiologists and surgeons in better managing respiratory dynamics.
For full details, refer to the original publication in Regional Anesthesia and Pain Medicine.
Da Conceicao D, Perlas A, Giron Arango L, et al. Validation of a novel point-of-care ultrasound method to assess diaphragmatic excursion. Reg Anesth Pain Med. 2024;49(11):800-804.
To learn more about the established methods of diaphragm assessment using POCUS, download NYSORA’s POCUS App today!