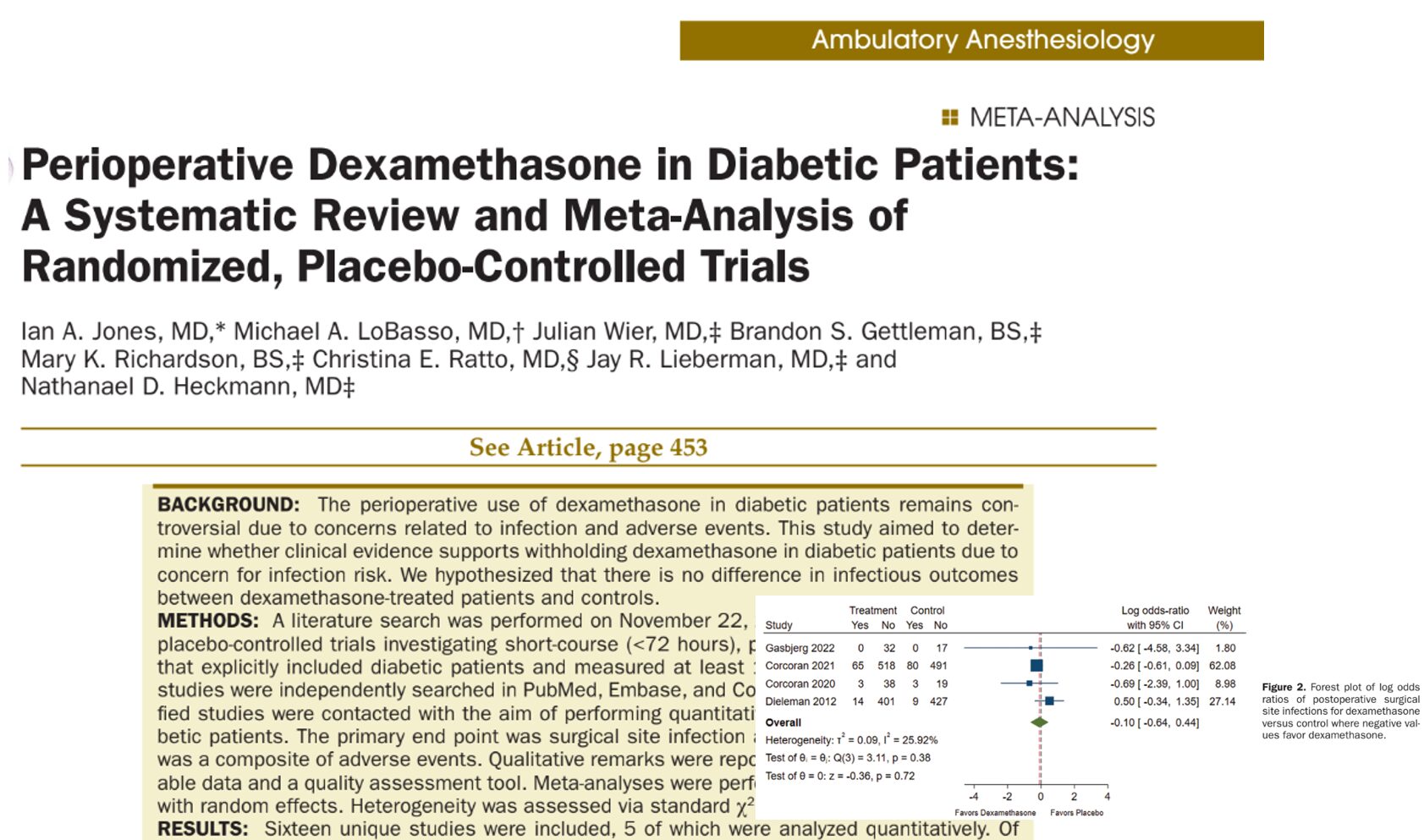
The relationship between diabetes mellitus (DM) and delayed gastric emptying has long been a concern for anesthesiologists, especially due to the associated risks of pulmonary aspiration during surgery. A recent study by Sastre et al., published in the December 2024 issue of Anesthesia & Analgesia, provides new insights into this issue by investigating the prevalence of full stomach in diabetic patients with and without dysautonomia compared to healthy controls. This landmark research highlights the importance of preoperative gastric ultrasound in risk assessment and management.
Key findings
Background
- Delayed gastric emptying is a common concern in diabetic patients due to potential autonomic dysfunction.
- Traditional fasting guidelines do not always account for individual variations in gastric emptying, particularly in diabetics.
Study overview
- Participants: 289 patients undergoing elective surgery:
- 83 diabetics with dysautonomia.
- 62 diabetics without dysautonomia.
- 144 healthy controls.
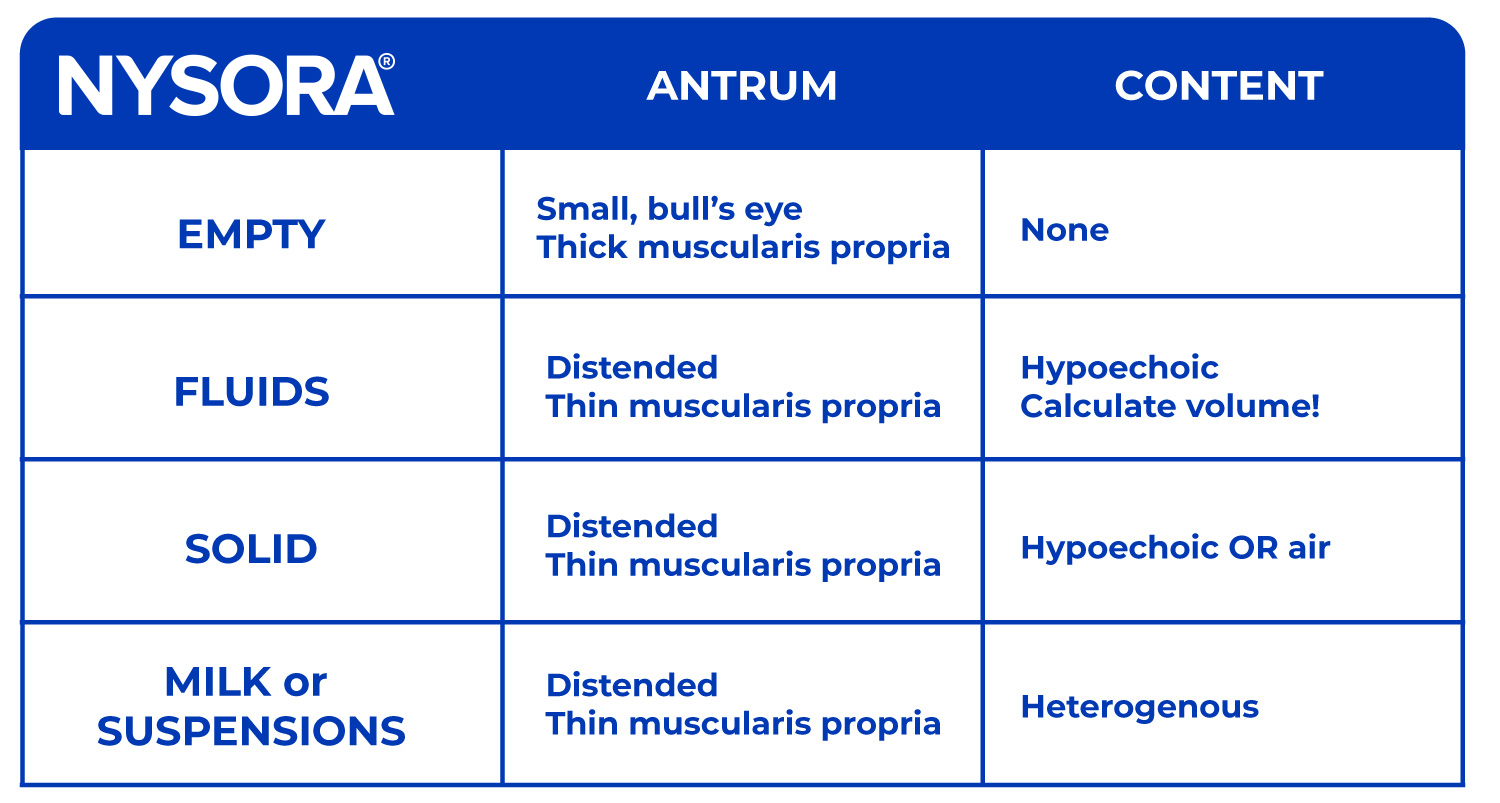
- Methodology: Preoperative gastric ultrasound was performed to assess gastric volume (GV) and content. The Perlas grading scale was used to classify gastric content.
Results
- Prevalence of full stomach:
- Higher in diabetic patients with dysautonomia (22.9%) compared to diabetics without dysautonomia (16.1%) and controls (13.2%).
- Solid gastric residue:
- Observed in 12% of diabetics with dysautonomia, compared to 4.8% in those without and 3.5% in controls.
- Gastric volume:
- While antral cross-sectional area (CSA) was larger in dysautonomia-positive diabetics, residual GV was not significantly different among groups.
- Gastroparesis symptoms:
- Common in diabetics with dysautonomia but not a definitive predictor of full stomach.
Implications for clinical practice
- Role of dysautonomia:
- The study underscores dysautonomia as a significant factor contributing to the presence of a full stomach, rather than diabetes alone.
- Utility of gastric ultrasound:
- Ultrasound is a reliable, non-invasive tool to assess gastric contents, enabling tailored perioperative management.
- Guideline reevaluation:
- Findings suggest that current fasting guidelines may not adequately address the unique risks in diabetics with dysautonomia.
Recommendations for anesthesia management
When to perform gastric ultrasound
- Patients with symptoms of dysautonomia or confirmed cardiovascular autonomic neuropathy.
- Uncertain fasting histories, especially in high-risk populations.
Interventions for positive findings
- Delay or cancel surgery if full stomach is detected.
- Consider pharmacological interventions, such as metoclopramide, to facilitate gastric emptying.
- Implement rapid sequence induction (RSI) or use regional anesthesia in selected cases.
Importance of individualized care
- Each patient should be assessed based on clinical history, symptoms, and diagnostic findings rather than relying solely on standard fasting durations.
Step-by-step guide: Performing gastric ultrasound
- Preparation:
- Position patient in supine and right lateral decubitus (RLD) positions.
- Use a curvilinear ultrasound probe (3–5 MHz).
- Scanning protocol:
- Supine position:
-
- Identify the gastric antrum using liver and aorta landmarks.
- Assess content type: empty, clear fluid, non-clear fluid, or solid.
- RLD position (if content is empty or clear in supine):
- If no content is visible, the stomach is empty (Grade 0).
- If fluid is visible, measure the cross-sectional area (CSA)
- Volume estimation:
- Measure the CSA of the gastric antrum three times and calculate the average.
- Apply Perlas’ formula to estimate gastric volume.
- Decision-making:
- Grade 0 or 1:
- Proceed with surgery.
- Grade 2 or solid content:
- Adjust plan based on urgency:
- Perform rapid sequence induction (RSI).
- Postpone/cancel surgery or evacuate stomach with a nasogastric tube.
- Modify airway management (e.g., supraglottic or endotracheal).
- Adjust plan based on urgency:
Conclusion
This study highlights the critical need for targeted risk assessments in diabetics, especially those with dysautonomia. Preoperative gastric ultrasound emerges as a game-changer, providing a practical solution to identify patients at risk for aspiration. As evidence mounts, integrating gastric ultrasound into standard perioperative care could significantly enhance patient safety and outcomes.
Learn more about gastric ultrasound with NYSORA’s POCUS App. Access clear, step-by-step instructions and practical tools to improve your ultrasound skills. Download now and get started!