Comparing baricity in spinal bupivacaine: Understanding its impact on hypotension during non-obstetric surgeries
Spinal anesthesia remains a cornerstone of anesthetic practice, particularly for lower limb and abdominal surgeries. Among the local anesthetics, bupivacaine is widely used for its potency and extended duration of action. However, the baricity of bupivacaine—its density relative to cerebrospinal fluid—can influence both its clinical effects and complications like hypotension. Therefore, Van Herreweghe et al. 2025 explored the impact of isobaric versus hyperbaric bupivacaine on hypotension in non-obstetric surgeries.
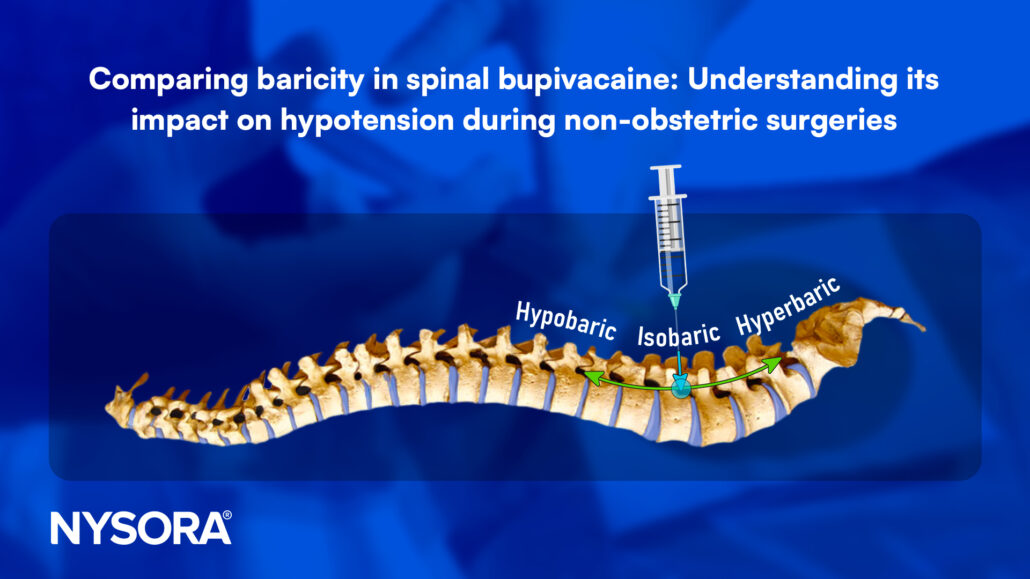
What is baricity?
- Baricity refers to the relative density of a solution compared to cerebrospinal fluid (CSF).
- Isobaric solutions: Similar density to CSF; spread less predictably, often confined near the injection site.
- Hyperbaric solutions: Denser, due to additives like glucose, tend to settle in dependent regions of the spinal canal, especially in specific patient positions.
Key findings from the review
The systematic review analyzed 10 randomized controlled trials encompassing 586 patients to compare isobaric and hyperbaric bupivacaine. While trends emerged, definitive conclusions were hampered by variations in methods, doses, and definitions of hypotension.
- Hypotension incidence:
- Most studies noted a higher incidence of hypotension with hyperbaric bupivacaine.
- However, no statistically significant difference was established overall.
- Hypotension occurred due to increased sympathetic blockade from the cephalad spread of hyperbaric solutions.
- Dose dependency:
- Studies predominantly used doses ≥15 mg, which may exaggerate effects not seen with lower, clinically relevant doses.
- Only one study used a low dose (5 mg) and found a possible link between hyperbaricity and hypotension.
- Patient positioning:
- The sitting position during administration showed a higher incidence of hypotension when hyperbaric solutions were used.
- Immediate changes to the supine position post-administration were common in studies, affecting the distribution of the drug.
- Sensory block levels:
- Hyperbaric bupivacaine resulted in higher sensory block levels (e.g., T4–T5) than isobaric solutions (e.g., T6–T8).
- Higher blocks led to more pronounced sympathetic blockade and hemodynamic changes.
Factors influencing outcomes
- Baricity and spread:
- Hyperbaric solutions demonstrate predictable spread in controlled positions but risk a more significant sympathetic blockade.
- Isobaric solutions are less predictable but may minimize hypotension due to limited cephalad spread.
- Standardization issues:
- Definitions of hypotension varied (e.g., systolic blood pressure drop ≥20% or below 90 mmHg), complicating comparisons.
- Variability in technique (e.g., spinal puncture level) and lack of ultrasound guidance introduced inconsistencies.
- Clinical relevance:
- Most trials used high doses that were unrepresentative of modern practices aimed at faster recovery.
- A lack of studies examining doses between 10–14 mg highlights the need for further research.
Implications for practice
Given the findings, several recommendations can be made:
- Patient selection:
- Hyperbaric bupivacaine may be ideal for procedures requiring high thoracic levels, while isobaric solutions may suit lower abdominal surgeries.
- Dosing considerations:
- Lower doses (<15 mg) should be explored for safety and effectiveness in current clinical practices.
- Technique optimization:
- Employ ultrasound guidance to ensure accurate puncture level and minimize variability.
- Monitoring:
- Standardized definitions of hypotension should be adopted, such as mean arterial pressure <65 mmHg or a drop >20% from baseline.
Future directions
This review underscores the heterogeneity in methodologies and the dated nature of many studies. To better understand the relationship between baricity and hypotension, future research should focus on:
- Standardized hypotension criteria.
- The impact of lower, clinically relevant bupivacaine doses.
- The role of patient positioning during and after administration.
- The use of ultrasound for precise spinal anesthesia delivery.
Conclusion
While trends indicate that hyperbaric bupivacaine may lead to a higher incidence of hypotension, statistically significant differences remain elusive due to variability in study designs. Nonetheless, patient positioning, dosing, and baricity-specific applications should be carefully considered to optimize outcomes.
For more information, refer to the full article in the European Journal of Anaesthesiology and Intensive Care.
Van Herreweghe, Imré; Ghysels, Eline∗; Gielen, Jens; Buck, Robbert; Flesher, Elizabeth; Cops, Jirka; Saldien, Vera; Mesotten, Dieter; Hadzic, Admir. Baricity of spinal bupivacaine and the incidence of hypotension in non-obstetric surgery: A systematic review. European Journal of Anaesthesiology and Intensive Care 4(1):p e0064, February 2025.
Learn more about spinal anesthesia with the Regional Anesthesia Manual e-Course. Access this valuable resource today on the NYSORA LMS website!