Comparing thoracic paravertebral block and stellate ganglion block for upper extremity sympathetic blockade
Chronic upper extremity pain, often caused by conditions such as complex regional pain syndrome (CRPS) and neuropathic pain, is notoriously difficult to treat. Sympathetic nerve blocks, including stellate ganglion block (SGB) and thoracic paravertebral block (TPVB), are widely used to provide relief by interrupting sympathetic nerve activity. However, the effectiveness of these two techniques in achieving sympathetic blockade remains debated. The presence of anatomical variations, such as Kuntz fibers, can result in treatment failures with SGB, raising interest in alternative approaches like TPVB. This study by Kim et al. (2025) compared ultrasound-guided TPVB and SGB to determine which technique provides a more successful sympathetic blockade and better pain relief in chronic upper extremity pain patients.
Study objective and methods
The primary objective of this study was to assess whether ultrasound-guided TPVB offers superior sympathetic blockade and pain relief compared to ultrasound-guided SGB.
- Design: A multicenter, prospective, randomized, open-label, comparative clinical trial.
- Participants: The study included 70 adult patients (aged 19–85) diagnosed with CRPS or neuropathic pain in the upper extremity. Patients were randomly assigned to receive either TPVB or SGB.
- TPVB group: Patients received a 10 mL injection of 1% mepivacaine at the T2 paravertebral space.
- SGB group: Patients received a 5 mL injection of 1% mepivacaine at the C6 level.
- Primary outcome: The success rate of sympathetic blockade, defined as a temperature increase of at least 1.5°C in the affected hand within 20 minutes after the procedure.
- Secondary outcomes: The temperature difference between the affected and unaffected hands, changes in peak systolic velocity (PSV) in the ipsilateral brachial artery, and pain scores at baseline, 20 minutes, 1 week, and 4 weeks after the procedure.
Key findings
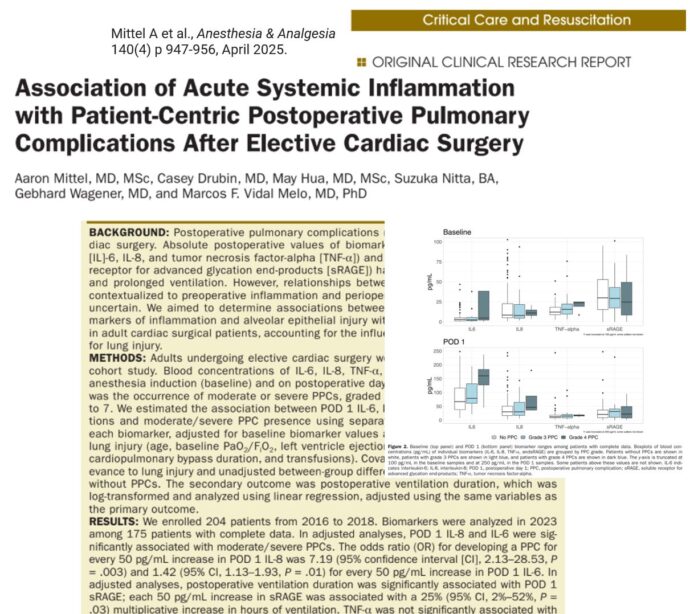
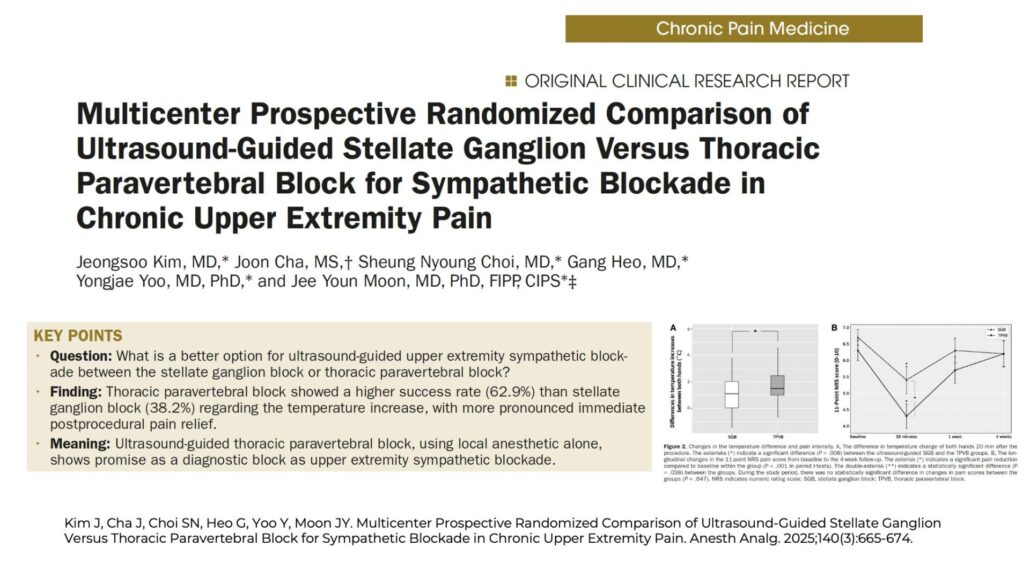
- Success rate of sympathetic blockade: TPVB was more effective, with a success rate of 62.9%, compared to 38.2% for SGB (P = 0.041). The difference in success rates was 24.6% (95% CI: – 9.0% to 58.2%), suggesting TPVB was significantly more effective in achieving sympathetic blockade.
- Temperature increase: The TPVB group experienced a greater increase in hand temperature (2.0°C ± 1.5) compared to the SGB group (1.1°C ± 1.3, P = 0.008), indicating a more pronounced sympathetic blockade.
- Pain reduction: Both groups experienced a significant reduction in pain at 20 minutes post-procedure (P < 0.001 for both). Patients in the TPVB group had a lower mean pain score (4.3 ± 2.2) compared to the SGB group (5.4 ± 2.4, P = 0.038). A greater proportion of TPVB patients (74.3%) experienced at least a 1-point pain reduction, compared to 47.1% in the SGB group (P =0.021).
- Follow-up pain scores: Pain relief was temporary in both groups, with pain scores returning to baseline at 1 and 4 weeks post-procedure. There was no significant difference in long-term pain relief between TPVB and SGB.
- Complications and side effects: Horner’s syndrome was more common in the SGB group (9 cases) compared to the TPVB group (3 cases). Hoarseness occurred in 7 SGB patients and 2 TPVB patients, resolving within 24 hours. No major complications, such as pneumothorax or respiratory distress, were reported in either group.
Conclusion
Ultrasound-guided TPVB demonstrated a higher success rate for upper extremity sympathetic blockade than SGB, with greater immediate pain relief and temperature increase. Additionally, TPVB was associated with fewer complications such as Horner’s syndrome and hoarseness. However, despite its superior initial effectiveness, the duration of pain relief was short-lived, as both groups showed a return to baseline pain levels by 1 and 4 weeks post-procedure. These findings suggest that while TPVB may be a better option for short-term pain relief, neither block alone provides sustained relief for chronic pain patients.
Future research
Future studies should investigate whether repeated TPVB procedures or combination treatments, such as adding neurolytic agents or corticosteroids, could prolong the duration of pain relief. Further research is also needed to compare TPVB with thoracic sympathetic ganglion blocks (TSGB) to determine the optimal technique for upper extremity sympathetic blockade. Large-scale, long-term studies will be critical in establishing evidence-based guidelines for managing chronic upper extremity pain using sympathetic blocks.
For more detailed information, refer to the full article in Anesthesia & Analgesia.
Kim J, Cha J, Choi SN, Heo G, Yoo Y, Moon JY. Multicenter Prospective Randomized Comparison of Ultrasound-Guided Stellate Ganglion Versus Thoracic Paravertebral Block for Sympathetic Blockade in Chronic Upper Extremity Pain. Anesth Analg. 2025;140(3):665-674.
Coming Soon: NYSORA’s US Pain Manual!
Keep an eye out for our upcoming US Pain Manual, a highly illustrated, step-by-step guide to ultrasound-guided chronic pain interventions. Whether you’re refining your technique or expanding your skill set, this resource will provide clear, practical guidance for precision pain management.