Learning objectives
- Recognize ARDS
- Treatment of ARDS
- Anesthetic management of ARDS
Definition and mechanism
- Acute respiratory distress syndrome (ARDS) is a life-threatening acute onset of respiratory failure
- Characterized by hypoxemia, stiff lungs, alveolar edema, endothelial cell damage, and neutrophil infiltration
- Multiple risk factors trigger the acute onset
- ARDS Berlin definition:
| Timing | Within 1 week of a known clinical insult or new or worsening respiratory symptoms |
| Chest imaging | Bilateral opacities - not fully explained by effusions, lobar/lung collapse or nodules |
| Origin of edema | Respiratory failure not fully explained by cardiac failure or fluid overload Need objective assessment (e.g. echocardiography) to exclude hydrostatic edema if no risk factor present |
| Oxygenation Mild Moderate Severe | 200 mmHg < PaO2/FiO2 ≤ 300 mmHg with PEEP or CPAP ≥ 5 cmH2O 100 mmHg < PaO2/FiO2 ≤ 200 mmHg with PEEP ≥ 5 cmH2O PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 cmH2O |
Signs and symptoms
- Severe shortness of breath
- Labored and unusually rapid breathing
- Low blood pressure
- Confusion and extreme tiredness
Risk factors
| Direct | Indirect |
|---|---|
| Pneumonia Aspiration of gastric contents Inhalation injury Pulmonary contusion Pulmonary vasculitis Drowning | Non-pulmonary Sepsis Major Trauma Pancreatitis Severe Burns Non-cardiogenic shock Drug overdose Multiple transfusions or Transfusion-related acute lung injury (TRALI) |
Complications
- Deep vein thrombosis
- Gastrointestinal bleeding
- Barotrauma
- Pneumothorax
- Nosocomial infection
- Delirium
- Pulmonary fibrosis
- Refractory respiratory failure requiring prolonged dependence on mechanical ventilation
- prolonged stay in ICU
- Need for tracheostomy
- Muscle weakness
- Sepsis
- Ambulatory dysfunction
Treatment
- Supplemental provision of oxygen
- Optimize PEEP: esophageal pressure, PV curves, lung ultrasound
- Protective mechanical ventilation
- Non-conventional therapies: prone position, high-frequency oscillatory ventilation, and extracorporeal membrane oxygenation
- Consider:
- Extracorporeal lung support (ECLS) techniques including ECMO as possible rescue therapy in patients with severe hypoxemic and hypercapnic respiratory failure
- Steroids: methylprednisolone
- Neuromuscular blocking agent cisatracurium or inhaled NO as these could improve oxygenation
Anesthetic management
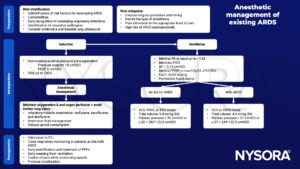
Volume-regulated volume control (VCV), pressure-regulated volume control (PRVC), or pressure-controlled (PCV) mode.
Hemodynamic management in ARDS
- Hemodynamic instability is often present in ARDS
- The right ventrile (RV) is most directly affected by positive-pressure mechanical ventilation and ARDS
- Therpaeutc strategies should be directed at preventing and treating RV dysfunction
- Optimize RV preload
- Optimize RV systolic function
- Reduce RV afterload
- Maintain an adequate systemic blood pressure and coronary perfusion
- Treat underlying disease
- Spectrum of pulmonary vascular dysfunction in acute respiratory distress syndrome (ARDS) and principal treatment strategies:
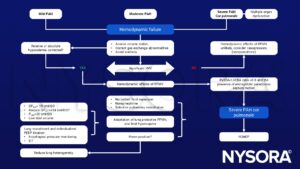
MOD, multiple organ dysfunction; PAH, pulmonary arterial hypertension; NE, norepinephrine; PPV, pulse pressure variation; PPMV, positive-pressure mechanical ventilation; RVEDA, right ventricular end-diastolic area, LVEDA, left ventricular end-diastolic area; DPAW, airway driving pressure; DPTP, transpulmonary driving pressure; PPLAT, plateau pressure; PEEP, positive end-expiratory pressure; EIT, electrical impedance tomography; ECMO, extracorporeal membrane oxygenation.
Suggested reading
- Battaglini D, Robba C, Rocco PRM, De Abreu MG, Pelosi P, Ball L. Perioperative anaesthetic management of patients with or at risk of acute distress respiratory syndrome undergoing emergency surgery. BMC Anesthesiol. 2019;19(1):153.
- DiSilvio B, Young M, Gordon A, Malik K, Singh A, Cheema T. Complications and Outcomes of Acute Respiratory Distress Syndrome. Crit Care Nurs Q. 2019;42(4):349-361.
- Robert Wise, David Bishop, Gavin Joynt & Reitze Rodseth (2018) Perioperative ARDS and lung injury: for anaesthesia and beyond, Southern African Journal of Anaesthesia and Analgesia, 24:2, 32-39.
- Cortes-Puentes GA, Oeckler RA, Marini JJ. Physiology-guided management of hemodynamics in acute respiratory distress syndrome. Ann Transl Med. 2018;6(18):353.
- Fanelli V, Vlachou A, Ghannadian S, Simonetti U, Slutsky AS, Zhang H. Acute respiratory distress syndrome: new definition, current and future therapeutic options. J Thorac Dis. 2013;5(3):326-334.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com

