Learning objectives
- Describe adrenocortical insufficiency
- Recognize the symptoms and signs of acute adrenal insufficiency
- Anesthetic management of a patient with adrenocortical insufficiency
Definition and mechanisms
- The adrenal glands of patients with adrenocortical insufficiency do not produce adequate levels of steroid hormones (i.e., glucocorticoids [cortisol), mineralocorticoids [aldosterone], and androgens)
- These hormones play an important role in blood pressure homeostasis, electrolyte and fluid balance, and metabolism
| Type | Mechanism |
|---|---|
| Primary adrenal insufficiency (Addison’s disease) | Deficient glucocorticoid secretion by the adrenal glands. The adrenal glands are directly affected, thus mineralocorticoid production is also reduced. |
| Secondary adrenal insufficiency | Deficient adrenocorticotropin hormone (ACTH) secretion by the pituitary gland and subsequent decreased adrenal stimulation. The adrenal glands are not directly affected, thus mineralocorticoid production is minimally impacted. |
| Tertiary adrenal insufficiency | Deficient corticotropin-releasing hormone (CRH) secretion by the hypothalamus, causing a downstream reduction in ACTH production and subsequently decreased adrenal stimulation. The adrenal glands are not directly affected, thus mineralocorticoid production is minimally impacted. |
Signs and symptoms
- Acute condition (Addisonian crisis): Abdominal pain, vomiting, dehydration, and hypotension (particularly postural)
- Chronic condition: Insidious onset with fatigue, anorexia, weight loss, and postural hypotension (salt and water loss)
- Increased pigmentation
- Hypoglycemia
- Hyponatremia
- Hyperkalemia
- Raised serum urea
- Disorientation
- Weakness
- Dizziness
- Cardiovascular collapse
- Muscle and joint pain
- Nausea, vomiting, diarrhea
Complications
- Addisonian crisis: Life-threatening situation resulting in hypotension, hypoglycemia, and hyperkalemia requiring emergency treatment (i.e., IV hydrocortisone and fluid support). It may result from undiagnosed or untreated Addison’s disease combined with sudden stress on the body (i.e., injury, infection, or illness).
- Autoimmune Addison’s disease may be associated with other autoimmune diseases (e.g., pernicious anemia and Grave’s disease)
Treatment
- Physiological replacement doses of corticosteroids for all types of adrenocortical insufficiency
- Adrenal crisis (acute) treatment
- IV fluids
- IV glucocorticoids (i.e., hydrocortisone) and mineralocorticoids (i.e., fludrocortisone)
- Supportive measures and correction of any additional issues (e.g., electrolyte abnormalities)
- Chronic adrenal insufficiency treatment
- Oral glucocorticoids (i.e., hydrocortisone, prednisone, methylprednisolone, or dexamethasone) to replace cortisol
- Oral mineralocorticoids (i.e., fludrocortisone) to replace aldosterone, if primary adrenocortical insufficiency
- Oral androgens (i.e., dehydroepiandrosterone) to replace androgens, if necessary
Symptoms of long-term steroid therapy
- Hypertension
- Skin atrophy
- Myopathy
- Arthritis
- Osteoporosis
- Coronary artery disease
- Secondary diabetes mellitus
- Suppressed immune response
- Impaired wound healing
Anesthetic considerations
- Potential life-threatening situation: Shock, dehydration, hypotension
- Physiological considerations
- Cardiovascular: Impaired myocardial contractility, arrhythmias secondary to hyperkalemia
- Volume status: Dehydration (2-3 L)
- Electrolyte imbalance: Hyperkalemia, hyponatremia (decreased level of consciousness, seizures), and hypoglycemia (decreased level of consciousness, seizures)
- Pharmacologic considerations
- Reduced circulating catecholamines (consider vasopressin for hypotension)
- Succinylcholine-induced hyperkalemia
Management
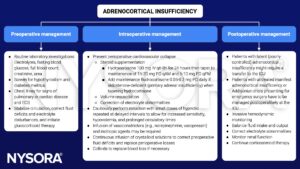
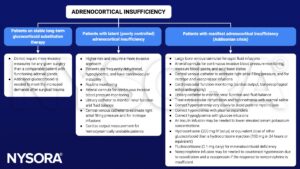
See also perioperative steroids considerations
Keep in mind
- Stress of surgery, infection, or trauma can cause adrenocortical insufficiency to decompensate and lead to an Addisonian crisis
- Prolonged steroid therapy can suppress the HPA axis without causing symptoms → symptoms manifest if the steroids are withheld or the dose is not adapted to increased requirements
- Patients on corticosteroid substitution therapy require a perioperative increase of the dose to compensate for the increased requirements posed by the trauma of surgery
- Patients with untreated adrenocortical insufficiency should not be scheduled for elective surgery until corticosteroid therapy has been given for a sufficient length of time
- Patients with untreated manifest adrenocortical insufficiency or Addisonian crisis presenting for emergency surgery are high-risk patients and require invasive intraoperative monitoring
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 6 Endocrine system.
- Davies MJ, Hardman JG. Anaesthesia and adrenocortical disease. Continuing Education in Anaesthesia. Critical Care & Pain. 2005;5(4):122-126.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com


