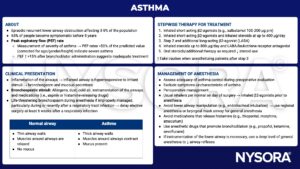
Learning objectives
- Manage patients with asthma in the pre-, and perioperative period
Definition
- Asthma is an airway condition characterized by variable respiratory symptoms and variable airflow limitation, typically, but not always, associated with airway inflammation and airway remodeling
- In between asthma attacks, a patient might be asymptomatic, and lung function tests might be normal
Symptoms
- Symptoms are nonspecific and include wheezing, shortness of breath, chest tightness, and cough
- The most characteristic features relate to the pattern of symptoms, including symptom nature, timing, triggers, and response to treatment
- Childhood-onset allergic asthma is commonly associated with atopy
- Late-onset asthma (> 12 years) is often non-atopic
- Exercise-induced bronchoconstriction might be the only symptom of asthma
Pathophysiology
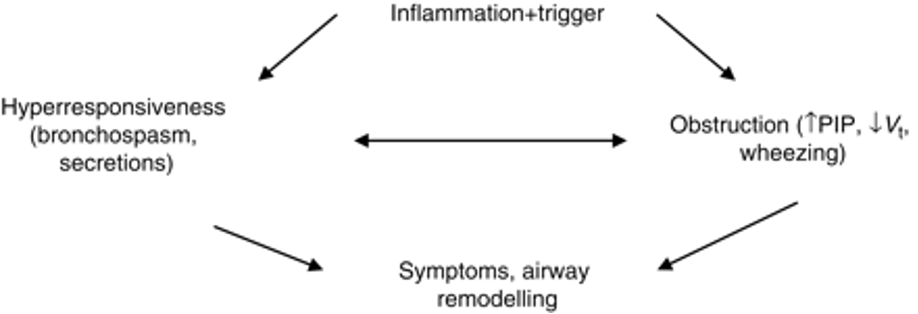
Pathophysiology of asthma and bronchospasm. PIP, peak inspiratory pressure, Vt, tidal volume. Adopted from Expert Panel Report 3 (EPR-3), from Elsevier.
Exacerbation treatment
- Exacerbations are characterized by progressively increasing shortness of breath, cough, wheezing or chest tightness, and decreasing lung function
- Onset is usually rapid in children but can develop over a week or more in adults
Acute exacerbation treatment
1. Give short-acting β2-agonists (SABAs) to resolve acute symptoms, they can be used every 15 to 20 minutes for the first hour
2. Add ipratropium bromide to decrease hospitalization rate and shorten ED stay for patients with severe or moderate asthma exacerbations
3. Give systemic corticosteroids as these decrease the rate of hospital admission, there is no difference between oral or i.v. corticosteroids
Preventative measures
4. A 5-day course of oral corticosteroids after ED treatment reduces the rate of relapse
5. A single dose of benralizumab, an anti-IL-5 receptor monoclonal antibody, reduces the rate and severity of subsequent exacerbations when given at the time of an initial exacerbation
Anesthesiological management
- Poorly controlled asthma poses a high additional risk for perioperative complications, well-controlled asthma confers almost no additional risk
- Question the patient on exacerbations, recent respiratory infections, and hospital visits
- Commerce strict smoking cessation as soon as possible
- Signs of acute bronchospasm or active lung infection should defer elective surgery
- Optimize medications and therapy compliance, consider a short course of oral methylprednisolone 40 mg for 5 days before surgery, as it has been shown to decrease post-intubation wheezing in newly diagnosed or poorly compliant patients with reversible airway obstruction
- Consider locoregional anesthesia where possible
- Give a short-acting bronchodilator prophylactically before surgery, ideally the patient’s own metered dose inhaler (MDI)
- Avoid bronchospasm
- Ensure adequate depth of anesthesia when manipulating the airway to avoid bronchospasm
- Consider using ketamine and/or sevoflurane which have a protective bronchodilating effect
- Don’t stimulate the airway (e.g., when suctioning) during emergence
- Practice good pain control
- Give preventive bronchodilator therapy
- Avoid bronchospasm
- Treatment of acute intraoperative bronchospasm
Suggested reading
- Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391(10122):783-800.
- Castillo JR, Peters SP, Busse WW. Asthma Exacerbations: Pathogenesis, Prevention, and Treatment. J Allergy Clin Immunol Pract. 2017;5(4):918-927.
- Woods BD, Sladen RN. Perioperative considerations for the patient with asthma and bronchospasm. BJA. 2009;103(1):i57-i65.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com