Learning objectives
- Definition of coagulopathy
- Management of coagulopathy
Definition and mechanisms
- Coagulopathy is a condition in which the blood’s ability to coagulate (form clots) is impaired
- Leading to a tendency toward prolonged or excessive bleeding and occurring spontaneously or following an injury
- Caused by:
- Genetic conditions such as hemophilia and Von Willebrand disease
- Acquired factors: anticoagulant medications (warfarin), the continued use of antibiotics, liver disease, or disseminated intravascular coagulation
- Activation of coagulation will lead to consumption of clotting factors, particularly factor V and fibrinogen, leading to a consumptive coagulopathy
Signs and symptoms
- Easy bruising
- Hemarthrosis (bleeding into a joint cavity)
- Hemorrhage after childbirth
- Accumulation of blood in the pleural cavity (hemothorax)
- Very heavy menstrual flow
- Loss of blood through the nose
- Anal bleeding
- Livedo reticularis
- Thrombocytopenia
- Gingival bleeding
- Rheumatisms
- Bloody gums
- Joint pain and swelling
- Blood in the urine
- Double vision
- Severe head or neck pain
- Repeated vomiting
- Difficulty walking
- Convulsions or seizures
Management
- Obtain a blood sample for a full coagulation screen
- Perform near-patient testing such as ROTEM or TEG
- Consider permissive hypotension in patients with moderate bleeding
- Perform massive volume resuscitation in a patient with severe hypovolemic shock
- Limit crystalloid and colloid infusions as this leads to acidosis, hypothermia and coagulopathy
- Transfuse red blood cells → hemoglobin target is between 7-9 dL/L
- Administer fresh frozen plasma, platelets, cryoprecipitate, and concentrated red cells, depending on clotting results and blood loss
- Correct hyperfibrinolysis with tranexamic acid (see also blood transfusion)
- Avoid volatile anesthetics as they lead to vasodilation
- Administer multimodal analgesia (opioids, NMDA glutamate receptor antagonists)
- Regional anesthesia is not indicated as it takes too much time and could mask compartment syndrome
- Avoid hypothermia as this worsens coagulopathy
- With passive rewarming, active external rewarming, and active internal rewarming
- Hypothermia impairs thrombin generation
- Hypothermia contributes to platelet dysfunction
- Consider complications associated with plasma administration such as TRALI, sepsis, and ABO incompatibility
Trauma-induced coagulopathy
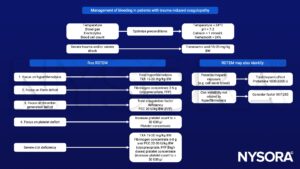
TXA, tranexamic acid; PCC, Prothrombin Complex Concentrates
Suggested reading
- Hofer S, Schlimp CJ, Casu S, Grouzi E. Management of Coagulopathy in Bleeding Patients. J Clin Med. 2021;11(1):1.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Simmons J, Powel M. 2016. Acute traumatic coagulopathy: pathophysiology and resuscitation. BJA: British journal of anaesthesia. 17;3:31-43.
- Gaunt, C., Woolley, T., 2014. Management of haemorrhage in major trauma. Continuing Education in Anaesthesia Critical Care & Pain 14, 251–255.
- Daniel Bolliger, Klaus Görlinger, Kenichi A. Tanaka, David S. Warner; Pathophysiology and Treatment of Coagulopathy in Massive Hemorrhage and Hemodilution. Anesthesiology 2010; 113:1205–1219.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com








