Learning objectives
- Describe congenital diaphragmatic hernia
- Understand the predictors for survival in congenital diaphragmatic hernia
- Management of congenital diaphragmatic hernia
Definition and mechanisms
- Congenital diaphragmatic hernia (CDH) is a birth defect characterized by the development of a hole in the diaphragm, leading to the protrusion of abdominal contents into the thoracic cavity affecting the normal development of the lungs
- 90% is left-sided
- Infants born with CDH experience respiratory failure due to pulmonary hypertension and pulmonary hypoplasia (decreased lung volume)
- Newborns born with CDH require immediate care at delivery → delivery should be as close to term as possible
- CDH is a life-threatening condition → death occurs due to
- Inadequate gas exchange surface
- Fixed high pulmonary vascular resistance (decreased vascular cross-sectional area, normal cardiac output)
- Reversible pulmonary hypertension
- Pneumothorax
- Additional anomalies (5%) and complications of intensive therapy
Diagnosis and survival
- CDH is usually discovered during a routine prenatal ultrasound
- The stomach, intestines, or liver may be present in the fetus’ chest where the lungs should be; the fetus’ heart may also be pushed to one side by the extra organs in the chest
Antenatal ultrasound predictors of survival in CDH
- Calculate the lung-to-head ratio (LHR) by dividing the fetal lung area (mm2) by the fetal head circumference (mm)
- LHR >1.35: 100% survival
- LHR 1.35 to 0.6: 61% survival
- LHR <0.6: No survival
- Calculate the observed to expected LHR (O/E LHR) by dividing the observed LHR by the expected ratio for gestational age
- The fetal lung area increases 16-fold compared to a 4-fold increase in the head circumference between 12 and 32 weeks of gestation
- O/E LHR <25%: Severe CDH (survival 10% with liver up and 25% with liver down)
- O/E LHR <15% with liver up: No survival
- Position of the liver (or presence of liver herniation)
- Liver herniation with LHR <1.0: 60% mortality
- Liver in the thorax: 56% survival
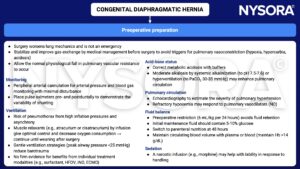
Anesthetic considerations
- Emergency situation
- Critically ill neonate
- Hypoplastic lungs
- Respiratory insufficiency (hypoxemia, hypercarbia, acidosis)
- Permissive hypercarbia may be required
- Consider HVO or ECMO
- Pulmonary hypertension
- Potential for right ventricle failure, reduced cardiac output
- Consider inhaled NO
- Transitional circulation
- Potential for right-left and left-right shunting
- Patent ductus arteriosus
- Delayed surgical repair, resuscitation is first priority
- NICU required
Management
Resuscitation
- Call NICU
- Indication for immediate tracheal intubation to facilitate intermittent positive pressure ventilation (IPPV)
- No bag-mask ventilation → distends herniated viscera, worsens mediastinal shift, and increases the risk of pneumothorax; while barotrauma further damages the hypoplastic lungs
- Nasal intubation helps with fixation and ventilator compliance
- Pass a nasogastric tube to deflate the gut and keep on free drainage
- Umbilical artery/vein lines
- ABG, chest X-ray, echocardiogram
- Lung protective ventilation
- Target SaO2 >85% and permissive hypercapnia (PaCO2 <65 mmHg, pH >7.25)
- PCV or PSV PIP <25 cmH2O
- Inspiratory time 0.35 sec
- PEEP 3-5 mmHg
- RR <65
- Consider HVO, iNO, or ECMO
- Consider NO and inotropes for pulmonary hypertension
- Fluid: Target MAP 45-50 mmHg
- Sedation: Opioids and benzodiazepines, thoracic epidural
- Avoid neuromuscular blocking drugs
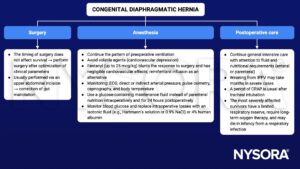
Keep in mind
- Immediate management at birth includes bowel decompression, avoidance of mask ventilation, and endotracheal tube placement if required
- The main focus of management includes gentle ventilation, hemodynamic monitoring, and treatment of pulmonary hypertension, followed by surgery
Suggested reading
- Leininger K, Chiu K. Anesthetic Considerations In Congenital Diaphragmatic Hernia. [Updated 2022 Nov 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572077/
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 24 Paediatrics, Lomas B.
- Chandrasekharan PK, Rawat M, Madappa R, Rothstein DH, Lakshminrusimha S. Congenital Diaphragmatic hernia – a review. Matern Health Neonatol Perinatol. 2017;3:6.
We would love to hear from you. If you should detect any errors, email us [email protected]