Learning objectives
- Describe the pathophysiology and clinical manifestations of cystic fibrosis
- Diagnose cystic fibrosis
- Manage patients with cystic fibrosis
Definition
- Cystic fibrosis is a multisystem autosomal recessive disease
- Most common lethal genetic disease in Caucasians
- Best considered as a disease spectrum rather than a distinct single clinical entity
Pathophysiology and clinical manifestations
| Site | Pathology | Clinical manifestation |
|---|---|---|
| Lower respiratory tract | Viscid mucous secretions, hypertrophy of goblet cells, decreased mucociliary clearance | Frequent LRTI, chronic hypoxaemia, cor pulmonale |
| Upper respiratory tract | Abnormal viscid nasal secretions | Sinusitis, nasal polyposis |
| Hepatobiliary system | Obstruction of bile ductules | Focal biliary cirrhosis, portal hypertension, multinodular biliary cirrhosis |
| Gastrointestinal tract | Abnormally viscid intestinal secretions at the level of the terminal ileum in the neonate | Meconium ileus, recurrent abdominal pain (distal intestinal obstruction syndrome) |
| Pancreas | Obstructed pancreatic ducts, fibrosis | Pancreatic exocrine insufficiency, CF-related diabetes (CFRD) |
| Reproductive system | Congenital absence of vas deferens, viscid cervical secretions | Infertility in men (98%), decreased fertility in women |
| Bone | Impaired calcium, vitamin D absorption, increased catabolism | Osteoporosis |
| Skin | Increased chloride levels | Abnormal ‘sweat test’, diminished thermoregulation |
Diagnosis
- Based on the presence of:
- One or more characteristic clinical features
Or
-
- History of cystic fibrosis in a sibling
Or
-
- Positive newborn screening (NBS) test
- PLUS laboratory evidence of an abnormality in the CF transmembrane conductance regulator (CFTR) gene or protein:
- Sweat testing: Transdermal administration of pilocarpine by iontophoresis to stimulate sweating and analysis of electrolyte concentrations
- Genetic testing
Treatment
- No curative treatment is available
- Treatment is supportive and aims to
- Minimize pulmonary infection
- Optimize nutritional status
- Slow disease progress
- Ease symptoms
| Respiratory | Physical therapy |
| Inhaled bronchodilators and mucolytics |
|
| Oscillatory devices, positive expiratory pressure devices, and high-frequency chest compression devices | |
| Oxygen therapy | |
| Pharmacologic | Mucolytics: DNA-ase, inhaled hypertonic saline |
| Anti-inflammatories: Oral corticosteroids, ibuprofen, azithromycin | |
| Antibiotics | |
| Nutrition | Enteral supplementation or parenteral nutrition |
| Subcutaneous insulin when needed | |
| Gene therapy | Under investigation |
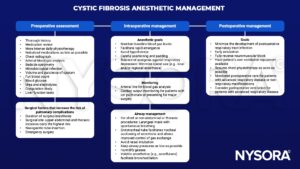
Anesthetic management
Suggested reading
- Fitzgerald M, Ryan D. Cystic fibrosis and anaesthesia. Continuing Education in Anaesthesia Critical Care & Pain. 2011;11(6):204-9.
- Huffmyer JL, Littlewood KE, Nemergut EC. Perioperative Management of the Adult with Cystic Fibrosis. Anesthesia & Analgesia. 2009;109(6).
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com