Learning objectives
- Define gastrointestinal reflux disease
- Describe the signs and symptoms of gastrointestinal reflux disease
- Anesthetic management of a patient with gastrointestinal reflux disease
Definition and mechanisms
- Gastroesophageal reflux disease (GERD) occurs when gastric content repeatedly and regularly flows back into the distal esophagus, this regurgitation (acid reflux) can irritate the lining of the esophagus
- Caused by frequent acid reflux or reflux of nonacidic content from the stomach due to inadequate closure of the lower esophageal sphincter (LES)
Signs and symptoms
Classic symptoms
- Heartburn (burning sensation in the chest), especially after eating, might be worse at night or while lying down
- Regurgitation (acid reflux)
- Taste of acid
- Upper abdominal or non-cardiac chest pain
- Globus
- Swallowing difficulties (dysphagia) and painful swallowing (odynophagia)
- Bad breath
- Bloating and belching
Extraesophageal symptoms
- Chronic cough
- Sore throat
- Dental corrosion
- Sinusitis
- Bronchitis
- Pulmonary fibrosis
- Recurrent aspiration pneumonia
- Hoarseness
- Hiccups
- Laryngitis
- Hypersalivation (water brash)
- New or worsening asthma
Complications
- Reflux esophagitis: Inflammation of the esophageal epithelium which can cause ulcer formation
- Esophageal stricture: Persistent narrowing of the esophagus caused by reflux-induced inflammation
- Barrett’s esophagus (precancerous changes to the esophagus): Intestinal metaplasia (changes of the epithelial cells from squamous to intestinal columnar epithelium) of the distal esophagus
- Esophageal carcinoma
Risk factors
- Obesity
- Hiatal or diaphragmatic hernia
- Pregnancy
- Connective tissue disorders (e.g., scleroderma)
- Delayed stomach emptying
Factors that exacerbate acid reflux
- Smoking
- Eating large meals or eating late at night
- Eating certain foods (e.g., fatty or fried foods)
- Drinking certain beverages (e.g., alcohol, coffee)
- Taking certain medications (e.g., aspirin, benzodiazepines, calcium channel blockers, tricyclic antidepressants, NSAIDs, and certain asthma medicines)
Treatment
- Lifestyle changes
- Avoid chocolate, mint, high-fat food, coffee, and alcohol
- Weight loss in overweight and obese patients
- Avoid bedtime snacks or lying down immediately after meals
- Avoid smoking
- Medications: Antacids, H2 receptor blockers, proton pump inhibitors (PPIs), prokinetics
- Surgery: Nissen fundoplication (the gastric fundus (upper part) of the stomach is wrapped around the lower end of the esophagus and stitched in place, reinforcing the closing function of the LES)
Management
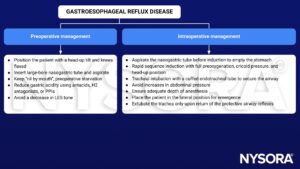
See also full stomach considerations
Keep in mind
- Patients with GERD are at an increased risk of pulmonary aspiration during anesthesia
- Factors that increase the risk of aspiration include the urgency of surgery, airway problems, inadequate depth of anesthesia, use of the lithotomy position, gastrointestinal problems, depressed consciousness, increased severity of illness, and obesity
- The main anesthetic goal in patients with GERD is to minimize regurgitation and aspiration of gastric contents
- Avoid drugs that decrease LES tone (e.g., opioids, anticholinergics, tricyclics, dopamine, and beta-agonists)
Suggested reading
- Jolliffe DM. Practical gastric physiology. Continuing Education in Anaesthesia Critical Care & Pain. 2009;9(6):173-177.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com