Learning objectives
- Define gestational diabetes
- Describe the complications associated with gestational diabetes
- Management of gestational diabetes
Definition and mechanisms
- Gestational diabetes is diabetes diagnosed for the first time during pregnancy, resulting in hyperglycemia affecting the pregnancy and baby’s health
- It can happen at any stage of pregnancy but most commonly develops in the second or third trimester
- Usually disappears after giving birth
- Occurs when the body cannot produce enough insulin to meet the extra needs in pregnancy
Signs and symptoms
Gestational diabetes does not usually cause any noticeable signs or symptoms
- Hyperglycemia
- Antenatal glycosuria
- Increased thirst
- More frequent urination
- Dry mouth
- Tiredness
- Blurred eyesight
- Genital itching or thrush
Complications
Maternal
- Gestational hypertension and pre-eclampsia
- Caesarean section
- Gestational diabetes in future pregnancies
- Type 2 diabetes
Fetal
- Excessive birth weight (i.e., >4.1 kg)
- Preterm birth
- Respiratory distress syndrome
- Hypoglycemia or jaundice
- Obesity and type 2 diabetes later in life
- Polyhydramnios
- Stillbirth
Risk factors
- Age >40 years
- Being overweight or obese (BMI >30 kg/m2)
- Prediabetes
- Gestational diabetes during a previous pregnancy
- Polycystic ovary syndrome
- Family history of diabetes
- Previously delivered a baby weighing ≥4.1 kg
- Black, Hispanic, American Indian, and Asian American ethnicity
Treatment
- Control blood glucose levels
- Changes in diet and being more active to lower blood glucose
- Medicine (i.e., tablets or insulin injections) if the above does not lower blood glucose enough
- Blood glucose testing kit to monitor the effects of treatment
- Close monitoring during pregnancy and birth to check for any potential complications
- Best to give birth before 41 weeks → induction of labor or caesarean section may be recommended if labor does not start naturally by this time
- Early delivery may also be recommended if there are health concerns for the mother or baby, or if the blood glucose levels are not well controlled
Management
- Goal: Avoid maternal hypoglycemia or hyperglycemia (which can increase the risk of neonatal hypoglycemia), safe management of glycemic control, effective analgesia for labor
- Availability of appropriate equipment to monitor and treat hypoglycemia or hyperglycemia (e.g., glucometer, infusion pumps, 20% glucose) in the delivery units and obstetric theaters
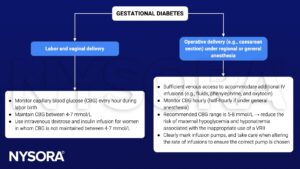
Variable rate intravenous insulin infusion (VRII) to maintain glycemic control
- Used when the target CBG range is not achieved by modification of the patient’s usual medications
- Glucose-containing substrate fluid alongside the IV insulin infusion to prevent gluconeogenesis, lipolysis, and ketoacidosis
- 5% glucose in 0.9% saline with premixed 0.15% (20 mmol/L) KCl or 0.30% (40 mmol/L) KCl to reduce the risk of developing hyponatremia
- Continue basal insulin after starting a VRII
See also pre-eclampsia considerations
See also caesarean section considerations
Prevention
- Eat healthy foods (high in fiber, low in fat and calories)
- Keep active
- Start pregnancy at a healthy weight
- Do not gain more weight than recommended during pregnancy
Suggested reading
- Yap Y, Modi A, Lucas N. The peripartum management of diabetes. BJA Educ. 2020;20(1):5-9.
We would love to hear from you. If you should detect any errors, email us [email protected]