Learning objectives
- Describe the pathophysiology and symptoms of hyperthyroidism
- Diagnose and treat hyperthyroidism
- Manage patients with hyperthyroidism or thyroid storm
Background
- Hyperthyroidism is a syndrome associated with excess thyroid hormone production
- Can lead to thyroid storm, an acute and life-threatening complication
- Most commonly caused by Graves disease (young population) and toxic multinodular goiter (older population)
- Other causes: Iodine-induced hyperthyroidism (Jod-Basedow phenomenon), thyroid adenomas, de Quervain thyroiditis (subacute thyroiditis), postpartum thyroiditis, factitious thyroiditis (thyrotoxicosis factitia)
Pathophysiology
- Graves disease
- Thyroid-stimulating antibodies mimicking the effects of thyroid-stimulating hormone (TSH)
- Typical signs: Edema of retro-orbital tissues, pretibial myxedema
- Toxic multinodaular goiter
- Palpable thyroid nodules leading to excess thyroid hormone production
- Thyroid adenoma
- Solitary palpable module causing hyperthyroidism
- Thyroiditis
- Transient increase in circulating thyroid hormone resulting from mechanical disruption of thyroid follicles
- Iodine-induced hyperthyroidism
- Typically iatrogenic
- Due to administration of iodine-containing medications (e.g., contrast media, amiodarone)
Signs & symptoms
- Weight loss despite increased appetite
- Palpitation
- Nervousness
- Tremors
- Dyspnea
- Fatigability
- Diarrhea
- Increased gastrointestinal motility
- Muscle weakness
- Heat intolerance
- Diaphoresis
- Goiter
- Palpable nodules
- Painful thyroid
Diagnosis
- Initial test: Serum TSH (decreased)
- Free T3 and T4 (increased)
- ECG when atrial fibrillation is suspected
- Palpitation of the thyroid gland
- 24-hour radioactive iodine (RAIU) uptake to distinguish between etiologies
- Increased RAIU: Graves disease, toxic multinodular goiter, thyroid adenoma
- Decreased RAIU: Subacute thyroiditis, painless thyroiditis, iodine-induced hyperthyroidism, factitious hyperthyroidism
- Thyroid receptor antibody measurement as an alternative diagnosis for Graves disease
- Radioisotope thyroid scan
Treatment
- Symptomatic
- Beta-blockers or calcium channel blockers
- Definitive
- Radioactive iodine
- Thionamide
- Subtotal thyroidectomy
- Clinical assessment and free T4 monitoring are essential for all treatments
Anesthetic management
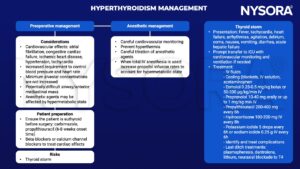
Keep in mind
- Acute coronary syndrome may be complicated with thyroid dysfunction
- Close monitoring is essential with propylthiouracil administration in pregnant patients as overcorrection can potentially cause fetal hypothyroidism
Suggested reading
- Pokhrel B, Aiman W, Bhusal K. Thyroid Storm. [Updated 2022 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448095/
- Mathew P, Rawla P. Hyperthyroidism. [Updated 2022 Jul 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537053/
- Carroll R, Matfin G. Endocrine and metabolic emergencies: thyroid storm. Ther Adv Endocrinol Metab. 2010;1(3):139-145.
- Farling PA. Thyroid disease. BJA: British Journal of Anaesthesia. 2000;85(1):15-28.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com