Learning objectives
- Define and classify the different types of hysterectomy
- Describe the complications that are associated with hysterectomy
- Management of a patient undergoing a hysterectomy
Definition and mechanisms
- A hysterectomy is the partial (cervix preserved) or total (cervix removed) surgical removal of the uterus
- It may also involve the removal of the cervix, ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures
- The woman can no longer get pregnant or menstruate after surgery
Classification
- Total or complete hysterectomy: Removal of the uterus and cervix, preserving the ovaries
- Supracervical or partial hysterectomy: Removal of just the upper part of the uterus while preserving the cervix
- Total hysterectomy with bilateral salpingo-oophorectomy: Removal of the uterus, cervix, fallopian tubes, and ovaries
- Radical hysterectomy with bilateral salpingo-oophorectomy: Removal of the uterus, cervix, fallopian tubes, ovaries, upper vagina, and some surrounding tissue (i.e., parametrium) and lymph nodes (cancer)
Indications
- Abnormal or heavy vaginal bleeding that is not managed by other treatments
- Severe pain with menstruation that is not managed by other treatments
- Leiomyomas or uterine fibroids (noncancerous tumors)
- Cervical or uterine cancer or abnormalities that may lead to cancer for cancer prevention
- Uterine prolapse
- Uterine hyperplasia, recurrent uterine polyps, endometriosis, or adenomyosis
- Postpartum to remove a severe case of placenta praevia or placenta percreta
- As a last resort in case of excessive postpartum hemorrhage
- Chronic pelvic pain related to the uterus but not managed by other treatments
Complications
- Blood clots (venous thromboembolism [VTE])
- Infection
- Heavy bleeding
- Urinary incontinence and vaginal prolapse
- Adhesion formation and bowel obstruction
- Torn internal stitches
- Urinary tract injury
- Vaginal problems
- Ovary failure
- Early menopause symptoms (e.g., hot flashes, vaginal dryness, loss of libido, insomnia)
- Issues related to anesthesia
Management
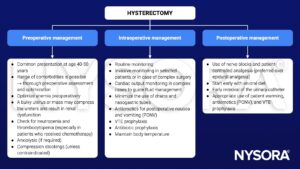
Techniques
| Technique | Advantages | Disadvantages |
|---|---|---|
| Abdominal hysterectomy | Not limited by the size of the uterus Combination with reduction and incontinence surgery possible No increase in postsurgical complications compared to vaginal technique | Longest recovery period and return to normal activities Higher risk of bleeding compared to laparoscopic surgery Vaginal or laparoscopic techniques are preferred in obese patients |
| Vaginal hysterectomy | Shortest surgery time Short recovery period and discharge from hospital Less pain medication compared to laparoscopic technique | Limited by the size of the uterus and previous surgery Limited ability to evaluate the fallopian tubes and ovaries |
| Laparoscopic-assisted vaginal hysterectomy | Possible with a larger uterus, depending on the surgeon's skills Combination with reduction operations are possible | Malignancies can only be removed by this approach if they are intact Not suggested for patients with cardiopulmonary disease |
| Total laparoscopic hysterectomy | Short inpatient treatment duration compared to abdominal technique Possiblity to diagnose and treat other pelvic diseases Quicker return to normal activities compared to abdominal technique Less bleeding, fevers, and infections compared to abdominal technique | Increased length of surgery Requires a high degree of laparoscopic surgical skills Higher risk of bladder or ureter injury |
Abdominal hysterectomy
- Trendelenburg position
- Transverse Pfannenstiel incision, occasionally midline incision
- General anesthesia or neuraxial block
- General anesthesia
- Muscle relaxation and controlled ventilation
- Adjustment of ventilation parameters due to diaphragmatic splinting caused by Trendelenburg position
- Multimodal analgesia with paracetamol, NSAIDs, opioids, and local blocks (e.g., TAP block for transverse incision, rectus sheath block for midline incisions)
- Neuraxial block
- Add an intrathecal opioid
- Block height to at least T4
- Do not position the patient for surgery too soon → Trendelenburg position will increase cephalad spread
- Manage hypotension with vasopressors
- General anesthesia
- Transfusion in patients with preoperative anemia
- Postoperative: Gabapentin, paracetamol, NSAIDs, opioids, patient-controlled analgesia, antiemetics, and VTE prophylaxis
Vaginal hysterectomy
- Lithotomy position → take precautions to avoid nerve injuries
- General anesthesia or neuraxial block
- General anesthesia
- Spontaneous breathing or mechanical ventilation → anticipate potential respiratory changes when the patient is moved into the Trendelenburg position
- Multimodal analgesia with paracetamol, NSAIDs, opioids, and local anesthetic infiltration
- Neuraxial block
- Consider adding an intrathecal opioid for postoperative analgesia
- Block height to at least T8
- Do not position the patient for surgery too soon → lithotomy and Trendelenburg position will increase cephalad spread
- Manage hypotension with vasopressors
- Supplemental sedation (if required)
- General anesthesia
- Less postoperative pain compared to abdominal technique
- Postoperative: Paracetamol, NSAIDs, oral opioids, antiemetics, and VTE prophylaxis
Laparoscopic hysterectomy
- Lithotomy position with steep Trendelenburg
- Consider the risk of pneumoperitoneum
- Large bore venous access to anticipate intraoperative cardiovascular complications or intraperitoneal injury
- Uterine manipulator is inserted through the cervix → may provoke vagal stimulation and bradycardia
- The uterus is removed vaginally (laparoscopic-assisted vaginal hysterectomy) or through an abdominal incision (total laparoscopic hysterectomy)
- General anesthesia
- Muscle relaxation, tracheal intubation, and controlled ventilation
- Pneumoperitoneum and steep Trendelenburg position will alter lung mechanics, and CO2 can accumulate from insufflation → adjust parameters to ensure adequate ventilation
- Multimodal analgesia with paracetamol, NSAIDs, opioids, and local infiltration
- Transfusion in patients with preoperative anemia
- Less postoperative pain compared to abdominal technique
- Postoperative: Paracetamol, NSAIDs, oral opioids, antiemetics, and VTE prophylaxis
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 11 Gynaecological surgery, Hobbs A and Craig SK.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com


