Learning objectives
- Outline the signs and symptoms of jaundice
- Describe the causes of jaundice and their classification
- Anesthetic management of a jaundiced patient
Definition and mechanisms
- Jaundice, or icterus, is a yellowish discoloration of the skin and sclera due to high bilirubin levels
- Jaundice in adults indicates the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary tract obstruction
- Surgery should be avoided in these patients, only emergency procedures
Signs and symptoms
- Hyperbilirubinemia (serum bilirubin ≥3 mg/dL)
- Yellowish discoloration of the skin, mucous membranes, and sclera
- Itchiness (pruritus)
- Pale fatty stool (steatorrhea)
- Dark urine (bilirubinuria)
- Abdominal pain
- Fatigue
- Weight loss
- Vomiting
- Fever
Complications
- Hyperbilirubinemia-induced neurological damage → kernicterus (especially in newborns)
- Coagulopathy
- Vitamin K-dependent coagulation factors (II, VII, IX, and X) are reduced, resulting in a prolonged prothrombin time
- Hepatocellular coagulopathy is often refractory to vitamin K administration
- Disseminated intravascular coagulation (DIC) is associated with secondary biliary tract infection
- Altered drug handling
- Drugs excreted via the biliary system have prolonged elimination half-life in cholestasis
- Atracurium is the drug of choice for muscular relaxation
- Acute oliguric renal failure (17%)
- Stress ulceration with gastrointestinal hemorrhage (16%)
- Reduced wound healing
Causes
| Category | Definition | Causes |
|---|---|---|
| Prehepatic/hemolytic | Pathology occurs prior to liver metabolism, due to increased breakdown of erythrocytes → increased rate of erythrocyte hemolysis → increased unconjugated serum bilirubin → increased deposition of unconjugated bilirubin into mucosal tissue | Sickle-cell anemia Spherocytosis Thalassemia Pyruvate kinase deficiency Glucose-6-phosphate dehydrogenase deficiency Microangiopathic hemolytic anemiaanemia Hemolytic-uremic syndrome Severe malaria |
| Hepatic/hepatocellular | Pathology is due to damage of parenchymal liver cells → abnormal liver metabolism of bilirubin | Acute hepatitis Chronic hepatitis Hepatotoxicity Cirrhosis Drug-induced hepatitis Alcoholic liver disease Gilbert syndrome Crigler-Najjar syndrome Leptospirosis |
| Posthepatic/cholestatic (obstructive jaundice) | Pathology occurs after bilirubin conjugation in the liver, due to obstruction of the biliary tract and/or decreased bilirubin excretion | Choledocholithiasis (common bile duct gallstones) Pancreatic cancer of the pancreatic head Biliary tract strictures Biliary atresia Primary biliary cholangitis Cholestasis of pregnancy Acute pancreatitis Chronic pancreatitis Pancreatic pseudocysts Mirizzi syndrome Parasites |
Risk factors
- Male gender
- White ethnicities
- Active smoking
Treatment
- Based on the underlying cause
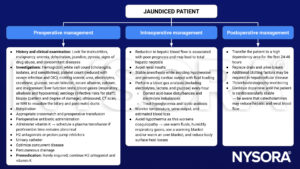
Management
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 4 Gastrointestinal tract, Jackson MJ.
- Wang L, Yu W. Obstructive jaundice and perioperative management. Acta Anaesthesiol Taiwan. 2014;52(1):22-29.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com