Learning objectives
- Describe Marfan’s syndrome
- Recognize signs and symptoms of Marfan’s syndrome
- Anesthetic management of a patient with Marfan’s syndrome
Definition and mechanisms
- Marfan’s syndrome (MFS) is an autosomal dominant condition of connective tissue, mainly involving the cardiovascular, musculoskeletal, and ocular systems
- MFS is caused by a mutation in the FBN1 gene on chromosome 15 that encodes the protein fibrillin
- The connective tissue abnormalities lead to connective tissue weakness with hyperextensible joints, eyes (dislocation of the lens), increased risk of valvular/aortic dissection, and spontaneous pneumothorax
Signs and symptoms
- Ocular: Lens dislocation, myopia, retinal detachment, glaucoma
- Cardiovascular: Aortic root dilatation with aortic regurgitation, aneurysm formation, aortic dissection, mitral valve prolapse with mitral regurgitation
- Musculoskeletal: Long bone overgrowth, scoliosis, kyphosis, joint hypermobility, pectus carinatum/excavatum, high-arched palate
- Respiratory: Spontaneous pneumothorax
- Skin: Striae
- Central nervous system: Dural ectasia
Complications
- Patients with MFS and left ventricular dilatation are at risk of ventricular arrhythmias
- Aortic root diameter >4 cm carries a risk of aortic dissection
Treatment
- Medications
- β-blockers
- Calcium channel blockers or ACE inhibitors if β-blockers are contraindicated/not tolerated
- Surgery to repair the aorta or replace a heart valve
Management
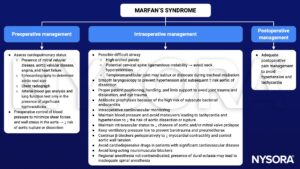
Obstetric anesthesia
- If no symptoms and aorta diameter <4 cm: No special considerations and vaginal delivery ok
- If aortic root dilation and aortic regurgitation: Multidisciplinary management with cardiology/cardiac surgery/obstetrics
- Some recommend caesarean section if aorta diameter >4.5 cm and labor if aorta diameter >4 and <4.5 cm
- Problems
- Airway might be even more difficult
- Neuraxial anesthesia for vaginal delivery and caesarean section
- Aortic dilatation with risk of dissection or rupture
- Perform monthly echocardiography during pregnancy
- Reduce shear forces on aorta
- Consider very early epidural placement
- Need for invasive monitoring
- Drug therapy to prevent hypertension and tachycardia (e.g., labetalol)
- Dural ectasia
- Higher risk for failed epidural, dural puncture, and postdural puncture headache
- Consider CT/MRI
Keep in mind
- Prevent a sudden increase in myocardial contractility, producing an increase in aortic wall tension, which could lead to aortic dissection
- Preexisting cardiovascular disease and the potential for acute cardiovascular and respiratory complications in patients with MFS require careful preoperative assessment and the use of a skillful anesthetic technique to avoid fatal complications
- Blood pressure control is the central component of perioperative management
Suggested reading
- Araújo MR, Marques C, Freitas S, Santa-Bárbara R, Alves J, Xavier C. Marfan Syndrome: new diagnostic criteria, same anesthesia care? Case report and review. Braz J Anesthesiol. 2016;66(4):408-413.
- Castellano JM, Silvay G, Castillo JG. Marfan Syndrome: Clinical, Surgical, and Anesthetic Considerations. Seminars in Cardiothoracic and Vascular Anesthesia. 2014;18(3):260-271.
- Allyn J, Guglielminotti J, Omnes S, Guezouli L, Egan M, Jondeau G, Longrois D, Montravers P. Marfan’s Syndrome During Pregnancy: Anesthetic Management of Delivery in 16 Consecutive Patients. Anesthesia & Analgesia. 2013;116(2): 392-398.
- Marfan Syndrome. In: Bissonnette B, Luginbuehl I, Marciniak B, Dalens BJ. eds. Syndromes: Rapid Recognition and Perioperative Implications. McGraw Hill; 2006. Accessed January 26, 2023.
We would love to hear from you. If you should detect any errors, email us [email protected]