Learning objectives
- Describe the pathophysiology of metabolic alkalosis
- Diagnose metabolic alkalosis
- Manage metabolic alkalosis
Background
- Metabolic alkalosis is defined as an increase in serum pH to >7.45
- Mostly due to a primary increase in serum bicarbonate (HCO3-)
- Associated with a secondary increase in CO2 arterial pressure (PaCO2)
- Usually accompanied by hypokalemia and hypochloremia
- Common aced-base disorder in critically ill patients
Pathophysiology
- Intracellular shift of hydrogen ions
- E.g. hypokalemia
- Decrease in serum hydrogen ions results in a relative increase in bicarbonate
- Renal loss of hydrogen ions
- Pathologies that increase the levels of mineralocorticoids or the effect of aldosterone lead to hypernatremia, hypokalemia, and hydrogen loss
- Loop and thiazide diuretics can induce secondary hyperaldosteronism
- Genetic defects leading to decreased expression of ion transporters in the loop of Henle (Bartter disease, Gitelman disease)
- Retention/addition of bicarbonate
- Overdose of exogenous sodium bicarbonate
- Compensatory mechanism for hypercarbia: hypoventilation and CO2 retention result in renal compensation over time by retaining bicarbonate (post-hypercapnia syndrome)
- Contraction alkalosis
- Occurs when a large volume of sodium-rich, bicarbonate low fluid is lost
- Diuretic use, cystic fibrosis, congenital chloride diarrhea
- Net concentration of bicarbonate increases
- Evaluation of etiology: Urinary chloride
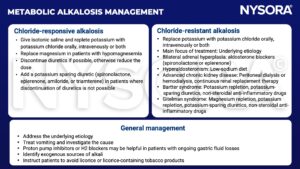
- Chloride responsive (urine chloride <10 mEq/L): Gastrointestinal hydrogen loss, congenital chloride diarrhea syndrome, contraction alkalosis, diuretic therapy, post-hypercapnia syndrome, cystic fibrosis, exogenous alkalotic agent use, villous adenoma, high volume ileostomy output
- Chloride resistant (urine chloride >20 mEq/L): Retention of bicarbonate, intracellular shift of hydrogen, hyperaldosteronism, Bartter syndrome, Gitelman syndrome, Cushing’s syndrome, exogenous mineralocorticoids, congenital adrenal hyperplasia, licorice, Liddle syndrome
- Adverse effects
- Decreased myocardial contractility
- Arrhythmias
- Decreased cerebral blood flow
- Delirium
- Increased neuromuscular excitability
- Impaired peripheral oxygen unloading
- Compensatory increase in arterial pCO2
- Net effect resulting in hypoxia
Diagnosis
- Elevated serum HCO3- and pCO2
- Determine respiratory compensation
- PaCO2 (mmHg) = 40 + 0.6 × (HCO3- – 24 mmol/l)
Management
Suggested reading
- Brinkman JE, Sharma S. Physiology, Metabolic Alkalosis. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482291/
- Tinawi M. Pathophysiology, Evaluation, and Management of Metabolic Alkalosis. Cureus. 2021;13(1):e12841. Published 2021 Jan 21.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com