Learning objectives
- Define multiple endocrine neoplasia syndromes
- Describe the differences between MEN type 1 and MEN type 2
- Anesthetic management of patients with multiple endocrine neoplasia syndromes
Definition and mechanisms
- Multiple endocrine neoplasia (MEN) syndromes are characterized by hyperplasia of or a tumor in specific endocrine system glands and tissues
- Caused by a genetic mutation, autosomal dominant inheritance
Classification
MEN type 1
- Genetic condition in which multiple tumors affect different aspects of the endocrine system
- Most common affected areas: Parathyroid glands, gastroenteropancreatic tract, and anterior pituitary gland
- Less common types of tumors: Neuroendocrine tumors of the thymus and bronchi, adrenocortical tumors, lipomas, visceral leiomyomas, truncal and facial collagenomas, facial angiofibromas, breast cancer, meningioma, ependymomas
- Most tumors are benign
- Tumors are due to the inactivation of the MEN 1 oncosuppressor gene located on chromosome 11q13
MEN type 2
- Genetic polyglandular cancer syndrome
- All patients develop medullary thyroid carcinoma and have an increased risk of developing other tumors affecting other endocrine glands
- Patients with MEN type 2 also develop one or both of the following conditions
- Tumors result from oncogenic point mutations of the c-Ret proto-oncogene located on chromosome 10cen-10q11.2
Signs and symptoms
- Symptoms vary depending on which glands are affected by the hyperplasia or tumor
- Hyperplasia or tumors cause the affected glands to produce and release more hormones than normal
- Symptoms vary from person to person
MEN type 1
| Tumor/condition | Incidence | Associated hormone | Symptoms |
|---|---|---|---|
| Hyperparathyroidism | 90% | Parathyroid hormone | Related to hypercalcemia Mild: Joint pain, muscle weakness, fatigue, depression, trouble concentrating, loss of appetite Severe: Nausea and vomiting, confusion and forgetfulness, increased thirst and frequent urination, constipation, bone pain |
| Gastrinomas | 40% | Gastrin | Abdominal pain, diarrhea, gastroesophageal reflux (acid reflux), peptic ulcers |
| Insulinomas | 10% | Insuline | Related to hypoglycemia Confusion, shakiness, sweating, hunger, anxiety, heart palpitations, temporary vision changes |
| Prolactinomas | 25% | Prolactin | Women: Changes in menstruation unrelated to menopause (i.e., irregular menstruation or amenorrhea), infertility, milky discharge from the nipples when not pregnant or breastfeeding (galactorrhea), decreased libido Men: Decreased libido, erectile dysfunction, infertility Large tumor: Nausea and vomiting, vision changes (i.e., double vision or decreased peripheral vision) |
MEN type 2
| Tumor/condition | Incidence | Associated hormone | Symptoms |
|---|---|---|---|
| Medullary thyroid carcinoma | 100% | Lump and pain in front of the neck, voice changes (e.g., hoarseness), coughing, trouble swallowing, dyspnea | |
| Pheochromocytomas | 50% | Epinephrine and norepinephrine | Hypertension, headache, excessive sweating, tachycardia, arrhythmia, feeling shaky |
| Hyperparathyroidism | 20% | Parathyroid hormone | Related to hypercalcemia Mild: Joint pain, muscle weakness, fatigue, depression, trouble concentrating, loss of appetite Severe: Nausea and vomiting, confusion and forgetfulness, increased thirst and frequent urination, constipation, bone pain |
Diagnosis
| MEN type 1 | MEN type 2 | |
|---|---|---|
| Diagnosis | At least two of the three endocrine tumors associated with the condition One of the associated tumors and a family history | Medullary thyroid carcinoma and pheochromocytoma and/or parathyroid enlargement (hyperplasia) or tumor (adenoma) |
| Tests | Blood tests to detect elevated levels of certain hormones - Hyperparathyroidism: Parathyroid hormone + hypercalcemia - Gastrinomas: Gastrin - Insulinomas: Insulin - Prolactinomas: Prolactine CT and MRI scans Genetic testing of MEN 1 gene | Blood tests to detect elevated levels of certain hormones - Medullary thyroid carcinoma: Calcitonin - Pheochromocytoma: Catecholamines - Hyperparathyroidism: Parathyroid hormone + hypercalcemia CT and MRI scans Genetic testing of RET gene |
Treatment
Dependent on what endocrine glands and organs are affected, treatment may include
- Medications to treat symptoms and counteract the side effects of excess hormones
- Surgery to remove tumors or entire affected glands (e.g., thyroidectomy, parathyroidectomy)
- Replacement hormones if an endocrine gland is surgically removed
- Cancer treatment (e.g., chemotherapy and radiation) in case of metastasis
Management
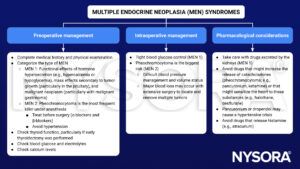
Anesthetic challenges per tumor
- Parathyroid tumors: Hypercalcemia
- Maintain hydration and urinary output
- Main risk: Potential for cardiac dysrhythmias
- Unpredictable responses to muscle relaxants
- Careful positioning due to the possible presence of osteoporosis and the potential for pathologic fractures
- Gastrinomas
- Correct hypovolemia and electrolyte imbalance (hypokalemia and metabolic alkalosis)
- Large gastric fluid volumes from gastric hypersecretion → vulnerable to aspiration during anesthetic induction
- Gastroesophageal reflux is common → rapid sequence induction with maintenance of cricoid pressure
- Insulinomas: Hypoglycemia
- Maintain normal blood glucose concentrations to prevent cerebral damage
- Place an intra-arterial catheter to measure glucose levels regularly
- Administer IV glucose
- Anesthetic technique should focus on agents that decrease the cerebral metabolic rate for oxygen (avoid ketamine)
- Maintain normocarbia during controlled ventilation
- Patients might be obese → pay attention to the airway and address respiratory and cardiac issues
- Maintain normal blood glucose concentrations to prevent cerebral damage
- Prolactinoma
- No specific anesthetic considerations
- Medullary thyroid carcinoma
- Enlarged thyroid causing airway compromise
- Intraoperative damage to the recurrent laryngeal nerve → may cause hoarseness, stridor, and complete airway obstruction upon extubation of the trachea or in the PACU
- Airway may also become compromised by hematoma formation compressing the trachea
- Pheochromocytoma: Hypertension
- Prevent hypertension and tachycardia → smooth anesthesia induction and endotracheal intubation
- Avoid catecholamine release induced by anesthetic or surgical maneuvers
- Correct hypovolemia and electrolyte imbalances
See also hyperparathyroidism considerations
See also pheochromocytoma considerations
Keep in mind
- The anesthetic course may range from routine with no special requirements to severe and life-threatening depending on the tumor
- Some syndromes demand specific management techniques, but a carefully and thoughtfully administered anesthetic is the key to a successful outcome in patients with MEN
Suggested reading
- Multiple Endocrine Neoplasia (MEN). In: Bissonnette B, Luginbuehl I, Marciniak B, Dalens BJ. eds. Syndromes: Rapid Recognition and Perioperative Implications. McGraw Hill; 2006. Accessed March 07, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=852§ionid=49517985
- Grant F. Anesthetic considerations in the multiple endocrine neoplasia syndromes. Curr Opin Anaesthesiol. 2005;18(3):345-352.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com


