Learning objectives
- Understand the impact of obesity and related health conditions upon the provision of anesthesia
- Identify the high-risk obese patient
- Plan safe and individualized perioperative care determined by comorbidities and the extent of surgery
Definition and mechanisms
- Obesity is an excessive fat accumulation that presents a risk to health, defined by the WHO as having a body mass index (BMI) over 30 kg/m2
- Obesity is a leading preventable cause of death worldwide
- The prevalence of obesity has tripled over the past 40 years, and there are more than 650 million obese adults worldwide
Risk factors
- Family inheritance and influences
- Lifestyle choices: Unhealthy diet, liquid calories, inactivity, sedentary lifestyle
- Certain diseases: Prader-Willi syndrome, Cushing syndrome, hypothyroidism, growth hormone deficiency, eating disorders (i.e., binge eating disorder, night eating syndrome)
- Certain medications: Antidepressants, insulin, sulfonylureas, thiazolidinediones, atypical antipsychotics, steroids, β-blockers, anticonvulsants (i.e., phenytoin and valproate), pizotifen, some forms of hormonal contraception
- Socioeconomic issues
- Aging
- Other factors: Pregnancy, quitting smoking, lack of sleep, stress, microbiome
Complications
- Hypertension
- Cardiovascular diseases and stroke
- Type 2 diabetes mellitus
- Metabolic syndrome
- Increased risk of cancer of the uterus, cervix, endometrium, ovary, breast, colon, rectum, esophagus, liver, gallbladder, pancreas, kidney, and prostate
- Digestive problems
- Obstructive sleep apnea (OSA)
- Obesity hypoventilation syndrome (OHS)
- Osteoarthritis
- Depression
Treatment
- Goal: Reach and stay at a healthy weight → improve overall health and lower the risk of developing complications related to obesity
- Initial treatment: Modest weight loss (5-10% of total weight)
- Changes in eating habits and increased physical activity
Dietary changes
- Reduce calories
- Eat healthier
- Restrict certain foods (e.g., high carbohydrates, full-fat foods)
- Feel full on less
- Meal replacements (e.g., low-calorie shakes or meal bars)
Exercise and activity
- Exercise: 150 minutes/week of moderate-intensity physical activity
- Keep moving
Behavior changes
- Counseling
- Support groups
Weight-loss medication
- Used along with diet, exercise, and behavior changes
- Bupropion-naltrexone
- Liraglutide
- Orlistat
- Phentermine-topiramate
Endoscopic procedures for weight loss
- Endoscopic sleeve gastroplasty
- Intragastric balloon for weight loss
- Limits the amount of food the patient can comfortably eat or decreases the absorption of food and calories
- May result in nutritional and vitamin deficiencies
- Adjustable gastric banding
- Gastric bypass surgery
- Sleeve gastrectomy
Management
Preoperative assessment and risk prediction
- Most important to identify
- Central or peripheral distribution of fat
- Presence of metabolic syndrome
- Peripheral oxygen saturation <95% breathing air
- Optimize associated health conditions before scheduling surgery (see table)
| Conditions | Suggestive features | Perioperative actions |
|---|---|---|
| Respiratory | ||
| Sleep-disordered breathing (OSA, OHS) | Shortness of breath SpO2 <95% breathing air Stop-BANG ≥5 OHS-BMI >30, hypercapnia when awake, raised HCO3, hypoxia, exclusion other causes of hypoventilation | ABG initially Spirometry CPET if abnormalities found in above tests Airway planning, 4x ↑ risk of difficult intubation and difficult mask ventilation Refer for further investigation and treatment Commence CPAP before surgery and continue after surgery BiPAP sometimes necessary for improvement in symptoms (especially OHS) Plan for postoperative HDU/ICU admission if symptoms not improved by time of surgery |
| Asthma | Dyspnea Wheezing | Asthmatic symptoms common but reversibility with β2-agonists not always found - cause is partly chronic pro-inflammatory state from excess adipose tissue and fat within/around chest/abdomen causing small airway collapse Weight loss: Symptoms from asthma and fat-related wheeze will improve |
| Cardiovascular | ||
| Hypertension Left ventricular hypertrophy Left ventricular failure Conduction abnormalities Cardiomyopathy | Clinical signs of heart failure History of cardiac syncope Increased SBP Reduced exercise capacity | Preoperative ECG ECHO if structural or functional disease suspected Referral to cardiologist Medical management and optimization before surgery |
| Right heart failure | Pulmonary hypertension resulting from sleep-disordered breathing Polycythemia |
|
| Reduced functional capacity | Difficult to assess in obese patients Ability to achieve 4 metabolic equivalents indicates fitness and low risk patient | Assess ability to walk on a flat level surface Assess climbing stairs CPET |
| Metabolic | ||
| Diabetes mellitus | Deranged serum glucose, HbA1C, or associated complications | Optimize glucose control with referral to endocrinologist Avoid delaying surgery based on HbA1C concentrations only |
| Liver involvement (NASH/NAFLD) | Evidence of cirrhosis, deranged liver function tests | Liver-shrinking diet (<1000 calories/day) can reverse the disease processes somewhat |
| Metabolic syndrome | Central obesity, hypertension, impaired glucose handing or diabetes, increased triglycerides, decreased HDL cholesterol | Actively seek components of metabolic syndrome (≥3 required for diagnosis) |
Organization and equipment
Preparation and positioning
- Ensure availability of theatre gowns of appropriate size
- Assess deep vein thrombosis risk and use prophylaxis measures
- Maintain patient’s dignity and safety
- Use gel pads to protect pressure points
Monitoring and ventilation
- Use non-invasive blood pressure cuffs of the correct size
- Anesthetic ventilators should be able to deliver high driving pressures and PEEP
- Potential for incomplete neuromuscular block antagonism requires routine neuromuscular monitoring
Ultrasound
- Facilitate successful regional blocks and aid with difficult venous access
Induction of anesthesia
Patient position
- Head up ramped position with elevation of the upper body until the ear tragus and sternal notch are aligned horizontally
- Position offers advantages
- Increased comfort for the patient
- Maintain functional residual capacity
- Reduce dyspnea
- Facilitate bag-mask ventilation
- Improve laryngoscopy
Airway
- Tracheal intubation is the recommended technique for airway management
- Obesity is associated with a higher risk of developing airway problems under anesthesia
- Routine airway assessment to determine potential difficult laryngoscopy or ventilation
- Mallampati score 3 (predicts difficult facemask ventilation and intubation)
- Neck circumference >42 cm (predicts difficult intubation)
- BMI >50 kg/m2 (independent predictor of difficult intubation and facemask ventilation)
- Symptoms of gastroesophageal reflux disease
- Obese patients have increased oxygen consumption and CO2 production due to increased total body tissue mass and increased work of breathing → can lead to hypercapnia and hypoxemia when ventilation is impaired
- Delay onset of hypoxemia by
- Preoxygenation of the lungs
- Induction of anesthesia in the semi-upright position with application of CPAP or high-flow nasal oxygen
- Avoid prolonged apnea
- Excess adipose tissue reduces chest wall compliance, which reduces functional residual capacity (FRC) to closing capacity, leading to atelectasis
Routine rapid sequence intubation (RSI)
- Obesity is associated with an increased incidence of known risk factors for aspiration (e.g., hiatus hernia, diabetes with autonomic neuropathy causing delayed gastric emptying)
- RSI is not routinely required in the absence of risk factors for aspiration
- Failed intubation after induction of anesthesia requires antagonism of neuromuscular block
Awareness
- Reduce awareness shortly after induction of anesthesia by
- Ensuring adequate dosing of i.v. anesthetic agents
- Prompt delivery of maintenance anesthetic agent
- Further i.v. bolus(es) of the anesthetic agent before airway manipulation or protracted airway maneuvers
Maintenance of anesthesia
- TIVA with propofol offers advantages over volatile anesthetics
- Reduced incidence of laryngospasm
- Reliable clearance of hypnotic agents
- Reduced postoperative nausea and vomiting
- Maintained anesthesia during protracted airway manipulation
- To minimize the risk of accidental awareness, the use of processed EEG-based depth of anesthesia monitoring, continuous clinical observation, and interpretation of vital signs should guide titration of drug infusion targets and rates
- Volatile anesthetics with a rapid offset of action (i.e., desflurane and sevoflurane) limit absorption into adipose tissue, reduce the risk of resedation, deteriorate respiration function, and may obstruct the airway at emergence
Ventilation
- Obesity is an independent risk factor for developing postoperative pulmonary complications
- Use lung protective volumes (6-8 mL/kg), plateau pressures <30 cm H2O, and titration of PEEP guided by the patient’s respiratory and cardiovascular state
- Position the patient in the 20° reverse Trendelenburg position with 45° hip flexion for laparoscopy for upper abdominal surgery to reduce airway pressures
- Position the patient in the flat Trendelenburg position for lower abdominal surgery to reduce airway pressures
Postoperative care
- Place the patient in a 30-45° head up position in the recovery room
- CPAP may enhance recovery of normal respiratory function if started in the early postoperative period
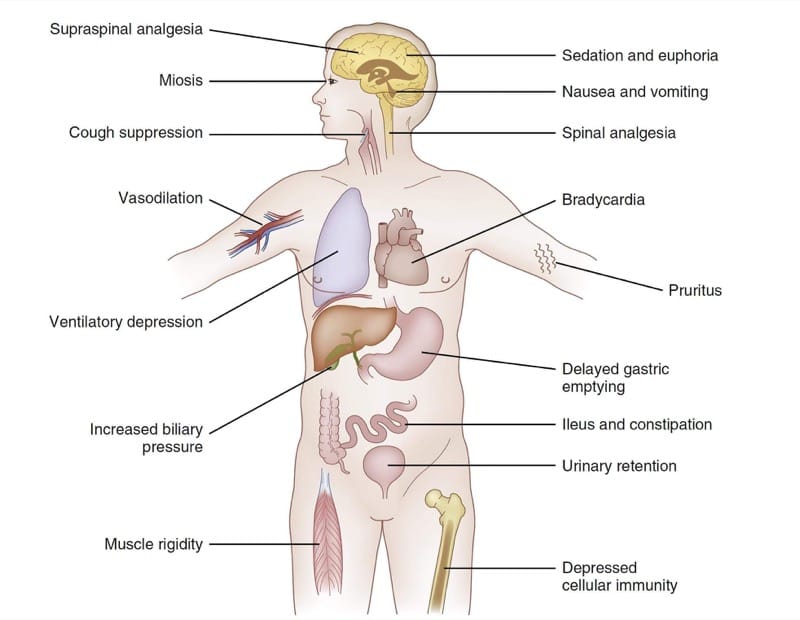
- Avoid opioids; if required monitor SpO2 continuously and consider a higher level of care
- Early mobilization with regular reviews
- Discharge criteria
- Unsupported stable vital signs with minimal inspired oxygen requirement
- No evidence of hypoventilation
- Free from apneas without stimulation
- Patient must be able to use a CPAP device if required
- Consider critical care admission for all patients with significant comorbidities (e.g., diabetes mellitus, chronic respiratory disease)
Day-case surgery
| Patient-specific factors | Anesthetic factors | Surgical factors | |
|---|---|---|---|
| Appropriate for day-case surgery | Any BMI Good functional capacity OSA/OHS effectively treated with CPAP/NIV Able to continue venous thromboembolism (VTE) prophylaxis at home if required | Adequate time on list to anesthetize Regional anesthesia possible Experienced anesthesiologist, OR, and day-case ward team | Adequate time on operating list to perform surgery, taking into account expected time to discharge Appropriate equipment for surgery and postoperative care available |
| Inappropriate for day-case surgery | Poor functional capacity Unstable hypertension, ischemic heart disease, congestive heart failure Unstable respiratory disease (low SpO2, OSA/OHS untreated or no symptomatic improvement after treatment) Previous VTE Metabolic syndrome | Likely to require long-acting potent opioids |
Implications of previous bariatric surgery
- Sleeve gastrectomy: Routinely intubate these patients as there is a risk of reflux of gastric contents, regardless of presence of symptoms
- Roux-en-Y gastric bypass; one anastomosis gastric bypass: May affect bioavailability of oral medications due to shortening of the small bowel and loss of surface area (e.g., postoperative analgesia absorption)
- Adjustable gastric banding
- High risk of aspiration despite prolonged fasting times
- RSI with antacid premedication should be routine
- Avoid nasogastric tubes unless acute abdomen or bowel obstruction (risk of displacing band or perforation of proximal stomach)
- The band should not be deflated (risk infection to system, band erosion in stomach or damage to the band)
Keep in mind
- Obesity only increases perioperative risk significantly when BMI is ≥40 kg/m2, or when associated with significant comorbidities
- Day-case surgery is usually appropriate if BMI is <50 kg/m2 and comorbidities are optimized
- OSA and OHS are common high-risk conditions that influence the management of anesthesia
- RSI should not be routine in the absence of specific indications
- Previous bariatric surgery has important implications for subsequent anesthesia
Suggested reading
- Seyni-Boureima R, Zhang Z, Antoine MM, Antoine-Frank CD. A review on the anesthetic management of obese patients undergoing surgery. BMC Anesthesiol. 2022; 22(98).
- Wynn-Hebden A, Bouch DC. Anaesthesia for the obese patient. BJA Education. 2020;20(11):388-395.
- Dority J, Hassan ZU, Chau D. Anesthetic implications of obesity in the surgical patient. Clin Colon Rectal Surg. 2011;24(4):222-228.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com