Learning objectives
- Anesthetic management of medical problems in obstetric patients
- Safe obstetrical general anesthesia
- Methods of pain relief during labor
Definition and mechanisms
- Pregnant women may need anesthesia at any stage of gestation due to incidental surgery (e.g. appendicitis), trauma, delivery, or complications in the immediate postnatal period (e.g. bleeding, breast abscess)
- As pregnancy progresses, multisystemic physiological changes develop rapidly
- The obstetric anesthesiologist must understand these to provide optimum care to pregnant women
- Consider:
- Significant cardiovascular or cerebrovascular disease
- Significant respiratory disease, which may worsen throughout pregnancy
- Morbid obesity (BMI >40) or super morbid obesity (BMI >50)
- Significant hematological disease which may previously have resulted in failure to reach viable gestation
- Corrected or palliated congenital heart disease
- Be aware that pregnant patients are more sensitive to the effects of general anesthesia than non-pregnant patients
Anesthetic management of medical problems in obstetric patients
- Acquired cardiac disease
- Ischaemic heart disease (obesity and advanced age is increasingly seen in the obstetric population)
- Aortic dissection
- Cardiomyopathy
- Symptomatic valvular heart disease
- Sudden adult death syndrome (SADS)
- Antenatal management:
- Assess symptoms and functional status (NYHA class)
- Review recent ECG and echocardiography
- Multidisciplinary planning for labor and delivery
- Labor and delivery:
- Perform continuous maternal monitoring with ECG and invasive blood pressure monitoring for high-risk patients
- Provide epidural analgesia
- Be aware of the hypertensive response to laryngoscopy in case of general anesthesia
- Postnatal management:
- Be cautious with uterotonic agents due to side effects
- Perform hemodynamic monitoring during the first 24 hours because of the risk of decompensation with autotransfusion postpartum
- Congenital cardiac disease
- Maintain preload
- Avoid prolonged fasting
- Administer IV fluids
- Maintain afterload
- Avoid spinal anesthetic
- Administer phenylephrine for hypotension (or noradrenaline in on-responders)
- Administer oxytocin slowly (2 units/minute)
- Avoid tachycardia
- Administer effective analgesia
- Perform early cardioversion for any tachyarrhythmia
- Keep pulmonary vascular resistance low
- Administer oxygen
- Avoid hypercarbia by preventing sedation
- Maintain preload
- Neurological disease
- Stroke
- Subarachnoid hemorrhage
- Epilepsy
- Status epilepticus
- Multiple sclerosis
- Consider a theoretical risk of neurotoxicity to demyelinated nerves with regional anesthesia
- Myasthenia gravis
- Perform instrumental delivery as muscles fatigue quickly
- Regional anesthesia is preferred over general anesthesia
- Avoid magnesium as it can precipitate a myasthenic crisis
- Multiple sclerosis
- Respiratory disease
- Asthma
- Screen for pulmonary hypertension
- Asthma
- Hematological disease
- Increased risk of VTE, e.g. Factor V Leiden, antiphospholipid syndrome
- Increased risk of bleeding, e.g. von Willebrand’s disease, thrombocytopenias
- Reduced oxygen-carrying capacity, e.g. sickle cell disease, thalassemia, spherocytosis
- Regional anesthesia is safe to use but pay attention to the timing of anticoagulant if used
- Therefore, provide a recent assessment of platelet count in thrombocytopenia
- Back problems
- Spinal surgery
- Regional anesthesia is safe to use in most types
- Avoid scar sites
- Scoliosis surgery
- Avoid regional anesthesia in women with implanted rods
- Spina bifida
- Exclude tethered spinal cord
- Regional anesthesia can be applied at an unaffected level if tethered spinal cord is excluded
- Be cautious of accidental dural punctures
- Reduce the epidural volume as dural permeability is reduced
- Spinal surgery
Maternal-to-fetal transfer
| Medication class | Examples | Crossing of uteroplacental barrier? |
|---|---|---|
| Intravenous agents | Thiopental Propofol Ketamine | Yes |
| Inhalational agents | Isoflurane Sevoflurane Desflurane | Yes |
| Benzodiazepines | Midazolam Lorazepam | Yes |
| Opioids | Morphine Fentanyl Remifentanil | Yes |
| Neuromuscular blocking agents | Vecuronium Rocuronium Suxamethonium | No |
| Neuromuscular blocking reversal agents | Neostigmine Sugammadex | Yes Yes |
| Anticholinergic agents | Atropine Glycopyrrolate | Yes Yes |
Obstetric general anesthesia
- Pre-OR preparation
- Airway assessment
- Fasting status
- Antacid prophylaxis
- Intrauterine fetal resuscitation if appropriate
- Rapid sequence induction
- Check airway equipment and IV access
- Optimize position: head up + left uterine displacement
- Pre-oxygenate and consider nasal oxygenation
- Perform cricoid pressure
- Deliver appropriate induction and neuromuscular blocker doses
- Consider facemask ventilation
- 1st intubation attempt:
- If poor view of the larynx, optimize the attempt by:
- Reducing/removing cricoid pressure
- External laryngeal manipulation
- Repositioning head/neck
- Using bougie/stylet
- Verify successful tracheal intubation or if the intubation attempt fails, ventilate with a facemask
- If poor view of the larynx, optimize the attempt by:
- 2nd intubation attempt:
- Consider:
- Alternative laryngoscope
- Remove cricoid pressure
- Verify successful tracheal intubation or if the intubation attempt fails, ventilate with a facemask
- Consider:
- Declare failed intubation:
- Priority is to maintain oxygenation
- Supraglottic airway device
- Facemask – oropharyngeal airway
- Priority is to maintain oxygenation
- Further management: see non-obstretic surgery
Pain relief during labor
- During the first and early second stages of labor, visceral pain (mediated by the T10 to L1 spinal segments) is experienced
- This is usually felt in the abdomen, sacrum, and back
- In the latter part of the first stage and into the second stage, somatic pain (mediated via T12-L1 and S2-4) is experienced
- This is located in the vagina, rectum, and perineum
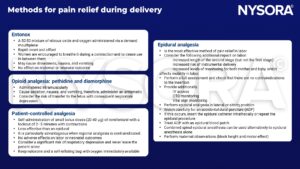
Methods for pain relief during labor
See caesarean delivery for anesthesia
Suggested reading
- Delgado, C., Ring, L., Mushambi, M.C., 2020. General anaesthesia in obstetrics. BJA Education 20, 201–207.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com

