Learning objectives
- Signs of placental abruption
- Degrees of placental abruption
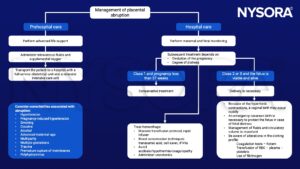
- Management of placental abruption
Definition and mechanisms
- Hemorrhage arising from the premature separation of a normally situated placenta
- Separation of the placental bed from the decidua basalis before delivery of the fetus
- Occurs in 1% of pregnancies
- Leading cause of vaginal bleeding in the latter half of pregnancy
- Emergency with high maternal and fetal morbidity/mortality
- Major complications:
- Hemorrhagic shock
- Acute kidney injury
- Coagulopathy
- Fetal demise
- Maternal death
- Delivering premature infant
- Transfusion-associated complications
- Hysterectomy
- Recurrence has been reported in 4 to 12% of cases
Signs and symptoms
- Key diagnostic factors:
- Vaginal bleeding (although about 20% of cases have no bleeding)
- Uterine tenderness
- Rapid contractions
- Abdominal pain
- Fetal heart rate abnormalities
- The clinical implications of a placental abruption vary based on the extent of the separation and the location of the separation
- Placental abruption can be complete or partial and marginal or central
- The classification of placental abruption is based on the following clinical findings:
Class 0: asymptomatic
Class 1: mild Class 2: moderate Class 3: Severe
Discovery of a blood clot on the maternal side of a delivered placenta
Diagnosis is made retrospectively No sign of vaginal bleeding or a small amount of vaginal bleeding
Slight uterine tenderness
Maternal blood pressure and heart rate within normal limits
No signs of fetal distress No sign of vaginal bleeding to a moderate amount of vaginal bleeding
Significant uterine tenderness with tetanic contractions
Change in vital signs: maternal tachycardia, orthostatic changes in blood pressure
Evidence of fetal distress
Clotting profile alteration: hypofibrinogenemia No sign of vaginal bleeding to heavy vaginal bleeding
Tetanic uterus/board-like consistency on palpation
Maternal shock
Clotting profile alteration: hypofibrinogenemia and coagulopathy
Fetal death
- Classification of 0 or 1 is usually associated with a partial, marginal separation
- Whereas, classification of 2 or 3 is associated with complete or central separation
Stages of hypovolemic shock
I Compensated II Mild III Moderate IV Severe
Blood loss <15%; 750–1000 ml 15–30%; 1000–1500 ml 30–40%; 1500–2000 ml >40%; ≥2000 ml
Heart rate (beats/min) <100 >100 >120 >140
Arterial pressure Normal; vasoconstriction redistributes blood flow, slight increase in diastolic pressure Orthostatic changes in arterial pressure, vasoconstriction intensifies in non-critical organs (skin, muscle, gut) Markedly decreased (systolic arterial pressure <90 mm Hg); vasoconstriction decreases perfusion to abdominal organs Profoundly decreased (systolic arterial pressure <80 mm Hg); decreased perfusion to vital organs (brain, heart)
Respiration Normal Mild increase Moderate tachypnea Marked tachypnea—respiratory failure
Mental status Normal, slightly anxious Mildly anxious, agitated Confused, agitated Obtunded
Urine output (ml/h) >30 20-30 <20 None (anuria)
Capillary refill Normal (<2 s) >2 s; clammy skin Usually >3 s; cool, pale skin >3 s; cold, mottled skin
Risk factors
- Health history and past obstetrical events:
- Smoking
- Cocaine use
- Maternal age over 35 years
- Hypertension
- Placental abruption in a prior pregnancy
- Current pregnancy:
- Multiple gestation pregnancies
- Polyhydramnios
- Preeclampsia
- Sudden uterine decompression
- Short umbilical cord
- Unexpected trauma
Causes
- The exact etiology is unknown
- Specific cause is often unknown
- Trauma or injury to the abdomen
- Rarely a short umbilical cord or rapid loss of amniotic fluid
Diagnosis
- Clinical signs/symptoms
- Ultrasound (however low sensitivity)
Management
Suggested reading
- Schmidt P, Skelly CL, Raines DA. Placental Abruption. In: StatPearls. Treasure Island (FL): StatPearls Publishing; April 1, 2022.
- Walfish, M., Neuman, A., Wlody, D., 2009. Maternal haemorrhage. British Journal of Anaesthesia 103, i47–i56.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







