Learning objectives
- Recognize the risk factors for PDPH
- Recognize signs and symptoms of PDPH
- Take measures to reduce the risk of PDPH
- Make diagnostic assessments for PDPH
- Manage PDPH occurrence
Definition & mechanisms
- Post-dural puncture headache (PDPH) is a headache occurring within 5 days of a dural puncture, caused by cerebrospinal fluid leakage through the puncture
- It is usually accompanied by neck stiffness and/or subjective hearing symptoms
- PDPH usually remits spontaneously within 2 weeks
Risk factors
- Patient-related:
- Age: Uncommon in patients less than 10 years of age; peak incidence is in the teens and early 20s
- Gender: Nonpregnant females have twice the risk compared to age-matched men
- Equipment related:
- Needle gauge (larger > smaller)
- Needle tip design (cutting > noncutting)
Risk management after accidental dural puncture
- Stylet Replacement
- Subarachnoid Saline
- Intravenous Cosyntropin
- Limiting/Avoiding Pushing during labor
- Intrathecal Catheters
- Epidural Saline
- Epidural Opiates
- Prophylactic Epidural Blood Patch
Signs & symptoms
- Most cases of PDPH will be typical in
- Onset—often delayed, but within 48 hours
- Presentation—symmetric, bilateral headache
- Associated symptoms—more likely with severe headache
- Symptoms:
- Headache accompanied by at least one of these symptoms:
- Neck stiffness
- Tinnitus
- Hypoacusia
- Photophobia
- Nausea
Diagnosis
- PDPH diagnosis remains a diagnosis of exclusion, it is critical to rule out other etiologies
- Benign etiologies
- Nonspecific headache
- Exacerbation of chronic headache (e.g., tension-type headache)
- Hypertensive headache
- Pneumocephalus
- Sinusitis
- Drug-related side effect
- Spontaneous intracranial hypotension
- Other
- Benign etiologies
-
- Serious etiologies
- Meningitis
- Subdural hematoma (SDH)
- Subarachnoid hemorrhage
- Preeclampsia/eclampsia
- Intracranial venous thrombosis (ICVT)
- Other
- Serious etiologies
Management
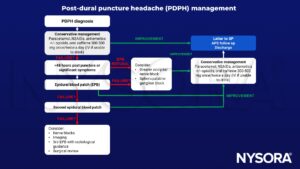
Keep in mind
- There is no evidence to support the common practice of recommending bed rest and aggressive hydration in the prevention of PDPH
- PDPH may carry a risk of medicolegal liability
- ADP may result in chronic headache and back pain
- Anesthetic procedures with risk of PDPH require proper informed consent
Suggested reading
- Statement on post-dural puncture headache management. American Society of Anesthesiologists (ASA). https://www.asahq.org. Published October 13, 2021. Accessed December 14, 2022.
- Russell R, Laxton C, Lucas DN, Niewiarowski J, Scrutton M, Stocks G. Treatment of obstetric post-dural puncture headache. Part 2: epidural blood patch. Int J Obstet Anesth. 2019;38:104-118
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com