Learning objectives
- Definition and signs and symptoms of pre-eclampsia
- Management of pre-eclampsia
Definition and mechanisms
- Pre-eclampsia is defined as new onset hypertension (systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or both) accompanied by one or more of the following features at or after 20 weeks of gestation:
- Proteinuria:
- Spot urinary protein creatinine ratio > 30 mg/mmol
- Or a 24-hour urine collection with > 300 mg of protein
- Other material organ dysfunction, including:
- Acute kidney injury
- Liver involvement
- Neurological complications: seizures, severe headaches, persistent visual scotomata, clonus, blindness, altered mental status, or stroke
- Hematological complications:
- Thrombocytopenia
- Disseminated intravascular coagulation (DIC)
- Hemolysis
- Proteinuria:
- Pre-eclampsia can be superimposed on women who have hypertension or proteinuria before 20 weeks of gestation and diagnosis can be more problematic in these patients
- Pre-eclampsia represents a potentially progressive clinical condition and the sub-categories ‘mild’ and ‘severe’ are no longer used
- HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome is potentially life-threatening to both mother and the baby and represents a severe form of pre-eclampsia
- Women may be critically unwell at presentation with placental abruption or DIC
- Left untreated, preeclampsia can lead to serious — even fatal — complications for both the mother and baby
- Early delivery of the baby is often recommended
- Pre-eclampsia affects 2–8% of pregnancies worldwide
Signs and symptoms
- Proteinuria or other signs of kidney problems
- Thrombocytopenia
- Increased liver enzymes
- Severe headaches
- Changes in vision, including temporary loss of vision, blurred vision, or light sensitivity
- Shortness of breath
- Abdominal pain
- Nausea or vomiting
Severe pre-eclampsia
- Severe features associated with pre-eclampsia that warrant consideration of planned early birth before 37 weeks of gestation:
- Inability to control maternal blood pressure despite using 3 or more classes of antihypertensives in appropriate doses
- Progressive deterioration in liver function, renal function, hemolysis, or platelet count
- Maternal pulse oximetry less than 90% on air
- Ongoing neurological features, such as severe intractable headache, repeated visual scotomata, or eclampsia
- Placental abruption
- Reversed end-diastolic flow in the umbilical artery Doppler velocimetry, a non-reassuring cardiotocograph or stillbirth
Causes
- Abnormal placentation
- Immunological factors
- Prior or existing maternal pathology (see risk factors)
- Dietary actors such as low dietary calcium intake
- Environmental factors such as air pollution
Risk factors
| High risk factors | Moderate risk factors |
|---|---|
| Hypertensive disease in previous pregnancy Chronic kidney disease Autoimmune disease (e.g. antiphospholipid syndrome) Type 1 or type 2 diabetes mellitus Chronic Hypertension | First pregnancy Age≥40 years Pregnancy interval≥10 yr Family history of pre-eclampsia Multiple pregnancy |
Prevention
- Daily intake of 75-150 mg aspirin from 12 weeks until 36-37 weeks of gestation for any woman with one high, or two or more moderate risk factors
- Calcium supplementation (> 1 g/day) in case of low calcium dietary intake
Diagnosis
- Blood pressure ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic on two separate readings taken at least four to six hours apart after 20 weeks of gestation in an individual with previously normal blood pressure
- An increase in systolic blood pressure of ≥ 30 mmHg or an increase in diastolic blood pressure of ≥ 15 mmHg in a woman with essential hypertension beginning before 20 weeks of gestational age
- Proteinuria ≥ 0.3 grams (300 mg) or more of protein in a 24-hour urine sample or a SPOT urinary protein to creatinine ratio ≥ 0.3
- Blood and urine analysis
- Fetal ultrasound
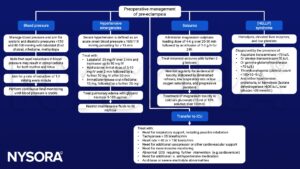
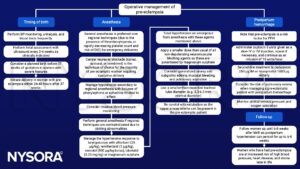
Management
Suggested reading
- Goddard, J., Wee, M.Y.K., Vinayakarao, L., 2020. Update on hypertensive disorders in pregnancy. BJA Education 20, 411–416.
- Leslie, D., Collis, R., 2016. Hypertension in pregnancy. BJA Education 16, 33–37.
We would love to hear from you. If you should detect any errors, email us [email protected]