Learning objectives
- Define and classify the different types of psoriasis
- Describe psoriasis triggers
- Anesthetic management of a patient with psoriasis
Definition and mechanisms
- Psoriasis is a chronic skin disorder characterized by an accelerated epidermal turnover and epidermal hyperplasia
- Autoimmune disease resulting from an increased rate of epidermal protein synthesis, rapid epidermal cell growth, shortened epidermal cell cycle, and increase in the proliferative cell population
- Lesions consist of sharply demarcated, loosely adherent, thickened, noncoherent, silver skin scales with increased vascularity → they most commonly appear on the extensor surfaces (i.e., elbows and knees), lumbar-sacral area, and scalp
- Injury to the skin can trigger psoriatic skin changes at that spot (Koebner’s phenomenon)
Classification
- Plaque psoriasis or psoriasis vulgaris
- Most common type (85-90%)
- Causes dry, itchy, raised skin patches (plaques) covered with scales
- Most commonly found on the elbows, knees, scalp, and back
- Nail psoriasis
- Affecting fingernails and toenails
- Causes pitting, abnormal nail growth, and discoloration
- Nails might loosen and separate from the nail bed (onycholysis)
- Guttate psoriasis
- Primarily affects young adults and children
- Triggered by a bacterial infection (e.g., strep throat)
- Marked by small, drop-shaped, scaling spots on the trunk, arms, or legs
- Inverse psoriasis
- Mainly affects the skin folds of the armpits, groin, buttocks, and breasts
- Causes smooth patches of inflamed skin that worsen with friction and sweating
- Fungal infections may trigger this type of psoriasis
- Pustular psoriasis
- Causes clearly defined pus-filled blisters
- Occur in widespread patches or on small areas of the palms or soles
- Erythrodermic psoriasis (erythroderma)
- Least common type
- Widespread inflammation and exfoliation of the skin over most of the body surface (>90% of the body surface area)
- Accompanied by severe dryness, itching, swelling, and pain
- Can develop from any type of psoriasis
Signs and symptoms
- Patchy rash ranging from spots of dandruff-like scaling to major eruptions across the entire body
- Rashes that vary in color (purple with gray scale to pink-red with silver scale)
- Small scaling spots
- Dry, cracked skin that may bleed
- Itching, burning, or soreness
- Cyclic rashes that flare for a few weeks or months and then subside
- Psoriatic lesions become colonized by bacteria (especially Staphylococcus aureus)
- Severe psoriasis may be associated with hyperuricemia, anemia, negative nitrogen balance, iron loss, and hypoalbuminemia
Complications
- Psoriatic arthritis, which resembles seronegative rheumatoid arthritis
- Temporary skin color changes (postinflammatory hypo- or hyperpigmentation) where plaques have healed
- Eye conditions (e.g., conjunctivitis, blepharitis, and uveitis)
- Obesity
- Diabetes type 2
- Hypertension
- Cardiovascular disease
- Other autoimmune diseases (e.g., ulcerative colitis, Crohn’s disease, celiac disease, or multiple sclerosis)
- Increased risk of developing non-melanoma skin cancer
- Mental health conditions (e.g., low self-esteem and depression)
Risk factors
- Genetic (HLA-Cw6)
- Family history
- Smoking
Psoriasis triggers
- Infections (e.g., strep throat or skin infections)
- Weather (cold and dry)
- Injury to the skin (e.g., cut or scrape, bug bite, or severe sunburn)
- Stress
- Smoking and exposure to secondhand smoke
- Obesity
- Heavy alcohol consumption
- Certain medications (e.g., lithium, beta-blockers, calcium channel blockers, antimalarial drugs, NSAIDs)
- Rapid withdrawal of oral or injected corticosteroids
Treatment
- Topical therapy
- Corticosteroids (i.e., hydrocortisone)
- Vitamin D3 analogs (i.e., calcipotriene and calcitriol) to slow skin cell growth
- Retinoids/vitamin A derivatives (i.e., tazarotene)
- Calcineurin inhibitors (i.e., tacrolimus and pimecrolimus) to calm the rash and reduce the scaly buildup
- Salicylic acid to reduce the scaling of scalp psoriasis
- Coal tar to reduce scaling, itching, and inflammation
- Anthralin to slow skin cell growth
- Phototherapy
- Sunlight
- UVB broadband and narrowband
- UVB
- PUVA
- Oral or injected (systemic) medications
- Corticosteroids
- Retinoids/vitamin A derivatives
- Biologics (i.e., apremilast, etanercept, infliximab, adalimumab, etc.) to suppress the immune system
- Methotrexate to decrease the production of skin cells and suppress inflammation
- Cyclosporine to suppress the immune system
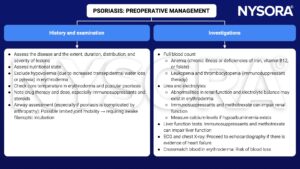
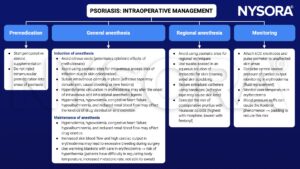
Management
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 9 Connective tissue, Lomas JP.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com