Learning objectives
- Describe Stevens-Johnson syndrome
- Understand the course of Stevens-Johnson syndrome
- Anesthetic management of a patient with Stevens-Johnson syndrome
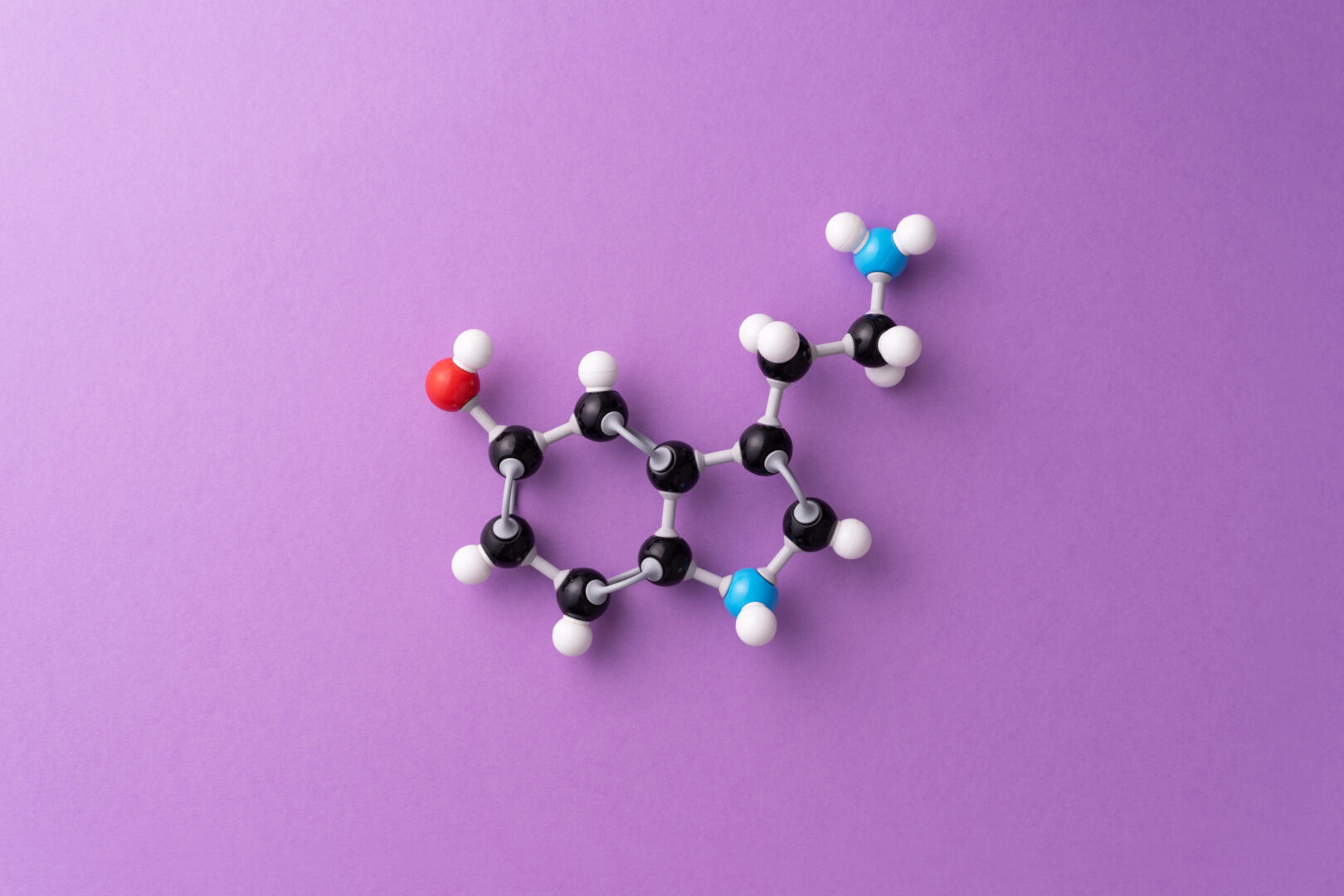
Definition and mechanisms
- Stevens-Johnson syndrome (SJS) is a rare, uncommon, and acute exfoliating disease of the skin and mucous membranes with systemic manifestations of variable severity
- SJS is a delayed-type hypersensitivity reaction in which SJS-inducing drugs or their metabolites stimulate cytotoxic T cells (i.e., CD8+ T cells) or T helper cells (i.e., CD4+ T cells) to initiate autoimmune responses
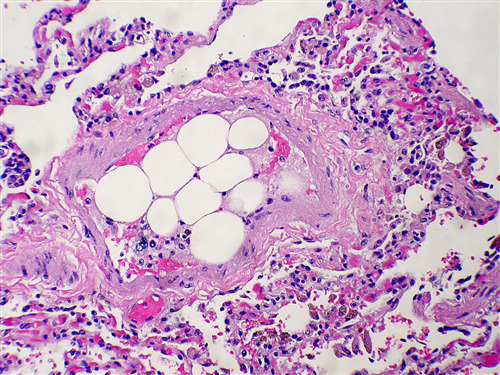
- The initial lesions of SJS are diffuse erythematous macules with purpuric, necrotic centers, and overlying blisters that may progress to skin slough, resulting in widespread superficial ulcers and loss of the epidermal barrier → fluid and protein loss → fluid and electrolyte imbalance with hypoproteinemia
Signs and symptoms
One to three days before a rash develops, early signs of SJS include
- Fever
- A sore mouth and throat
- Fatigue
- Burning, red eyes
As the condition develops, other signs and symptoms include
- Unexplained widespread skin pain
- A red or purple rash that spreads
- Blisters on the skin and mucous membranes of the mouth, nose, eyes, and genitals
- Shedding of skin within days after blisters form
Causes
- Infections (e.g., pneumonia and HIV)
- Drug-induced
- Anti-gout medications (e.g., allopurinol)
- Medications to treat seizures and mental illness (e.g., anticonvulsants and antipsychotics)
- Antibacterial sulfonamides (e.g., sulfasalazine)
- Nevirapine
- Pain relievers (e.g., acetaminophen, ibuprofen, and naproxen sodium)
- Malignancy-related
- Idiopathic
Risk factors
- HIV infection
- Weakened immune system: Organ transplant patients, HIV/AIDS, and autoimmune disease (e.g., systemic lupus erythematosus)
- Cancer: Particularly blood cancer
- History of SJS
- Family history of SJS
- Genetic factors
Complications
- Dehydration
- Sepsis
- Eye problems (e.g., eye inflammation, dry eye, and light sensitivity)
- Pneumonia
- Acute respiratory failure
- Permanent skin damage
- Multiple organ failure
Treatment
- Treatment requires hospitalization, in an ICU or burn unit
- Stop nonessential medications → stop taking SJS-inducing drugs
- Fluid replacement and nutrition
- Wound care
- Eye care
- Temperature management
- Medications
- Pain medications to reduce discomfort
- Medication to reduce inflammation of the eyes and mucous membranes (e.g., topical steroids)
- Antibiotics to control infection, when needed
- Other oral or i.v. medications (e.g., corticosteroids)
Management
- Maintain skin and mucous membrane integrity
- Minimize handling and transfer of patients to prevent further epithelial damage or rupture of bullae
- Safe airway management
- Mucous membranes of the respiratory tract and pleura may be involved
- Ulcers in the nose, oropharynx, trachea, and bronchi increase the risk of hematemesis
- Avoid manipulation and trauma to the oral, tracheal, and laryngeal mucosa (lesions are often present)
- Avoid desquamation of the skin on the face during mask pre-oxygenation
- Difficulties getting venous access, application of monitors and anesthesia face masks, airways, laryngoscopy, and intubation
- Establish access over areas of normal epidermis
- Use invasive BP monitoring
- Use one smaller than the standard size for laryngeal mask airways
- Adhere to strict aseptic precautions at all stages (immune-compromised state and susceptibility to respiratory infection)
- Induction with etomidate or ketamine could provide better hemodynamic stability when compared to propofol or thiopental
- Non-depolarizing muscle relaxants are often used if muscle relaxation is necessary to avoid succinylcholine and the associated risk of hyperkalemia
- Fluid and electrolyte replacement
- Avoid hypothermia
- OR temperature 28°C
- Warm i.v. fluids
- Water mattresses/forced air-warmers
- Adequate postoperative analgesia
Keep in mind
- Proper preoperative evaluation, identification of the precipitating agents in order to avoid them, a continuation of preoperative medications, and other immunosuppressants or steroids is essential
- Extreme care should be taken while transferring patients with fresh lesions
- Patients with involvement of the respiratory tract and pleura require special attention, including the application of a face mask, laryngoscopy, intubation, and suction with extra lubrication when general anesthesia is chosen
- Anesthetic drugs can be safely used in SJS patients
Suggested reading
- Ramsali MV, Puduchira KG, Maganti SP, Vankaylapatti SD, Pasupuleti S, Kulkarni D. Anesthetic management and outcomes of patients with Steven-Johnson Syndrome-A retrospective review study. J Anaesthesiol Clin Pharmacol. 2021;37(1):119-123.
- Kwass WK, Chow J. Anesthetic Management in Stevens-Johnson syndrome: Case Report. Integr Anesthesiol. 2019;2(1):001-004.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com