Learning objectives
- Describe systemic lupus erythematosus
- Understand the potential complications associated with systemic lupus erythematosus
- Anesthetic management of a patient with systemic lupus erythematosus
Definition and mechanisms
- Systemic lupus erythematosus (SLE) is a chronic autoimmune connective tissue disorder with a heterogeneous presentation and systemic involvement in which tissues and multiple organs are damaged by pathogenic autoantibodies and immune complexes
- There are often periods of illness (flares) and periods of remission during which there are few symptoms
Signs and symptoms
- Fatigue
- Fever
- Joint pain, stiffness, and swelling
- Butterfly-shaped rash on the face that covers the cheeks and bridge of the nose or rashes elsewhere on the body
- Skin lesions that appear or worsen with sun exposure
- Fingers and toes that turn white or blue when exposed to cold or during stressful periods
- Shortness of breath
- Chest pain
- Dry eyes
- Photosensitivity
- Headaches, confusion, and memory loss
- Hair loss
- Mouth ulcers
- Swollen lymph nodes
Risk factors
- Gender: Female > male
- Age: 15-45 years
- Race: More common in African Americans, Hispanics, and Asian Americans
Causes
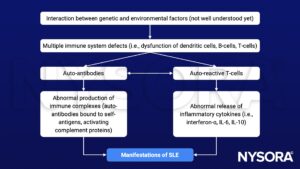
SLE is probably caused by a genetic susceptibility coupled with an environmental trigger, resulting in a defect in the immune system
- Genetics: Mutations in HLA-DR2/HLA-DR3 genes, complement genes, cytokine genes, etc.
- Environmental: UV-light (UV-A, UV-B), viruses (e.g., EBV, CMV, retroviruses), drugs (e.g., minocycline, hydralazine, procainamide), hormones (e.g., estrogen, prolactin), heavy metals
Complications
- Dermatologic: Malar rash, chronic discoid lesions
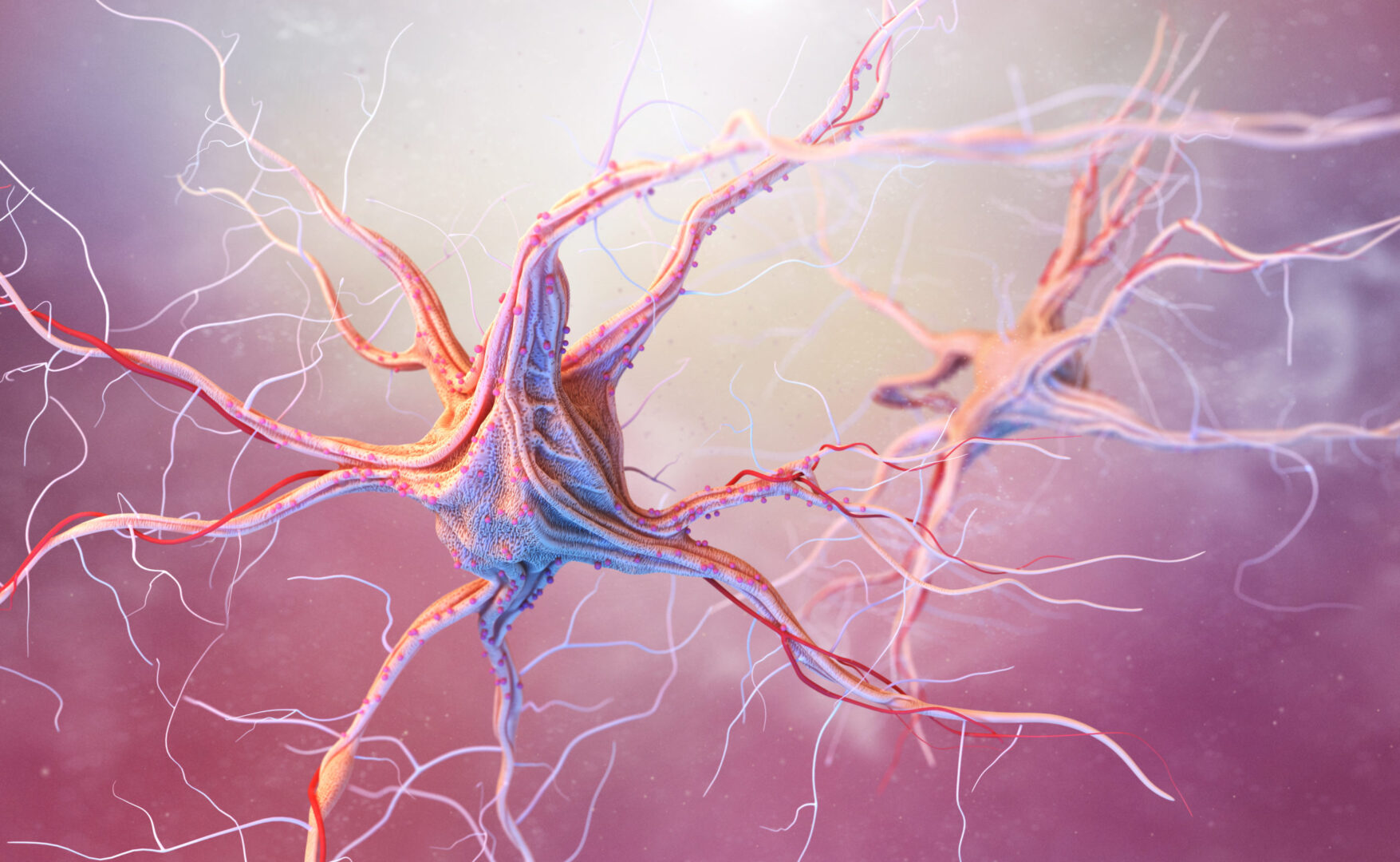
- Brain and central nervous system: Headaches, dizziness, behavior changes, vision problems, strokes or seizures
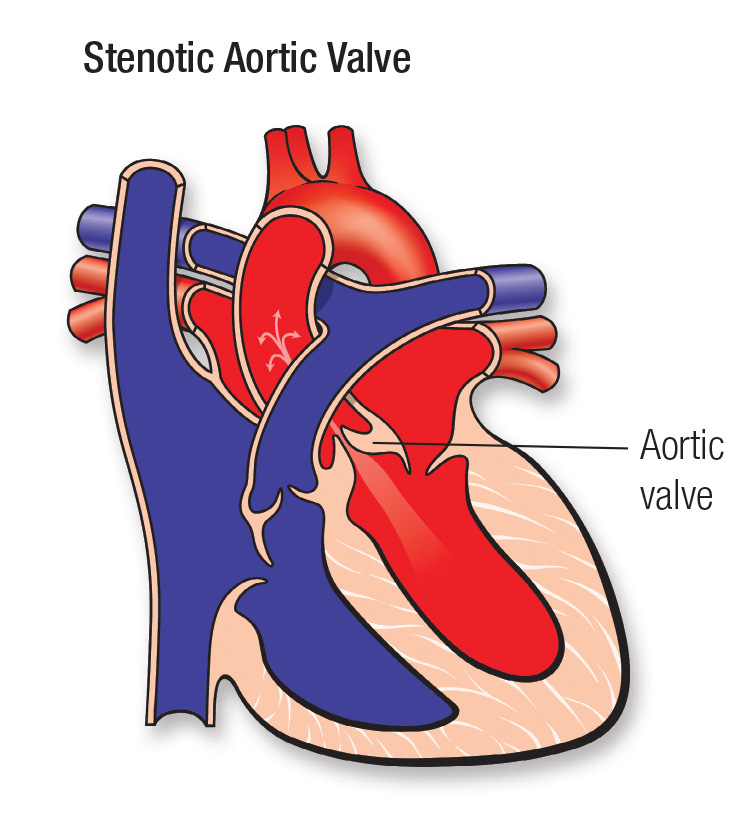
- Cardiovascular: Symptomatic pericarditis, pericardial tamponade, myocarditis, Libman-Sacks endocarditis, valvular dysfunction, Raynaud’s phenomenon
- Pulmonary: Pleuritis, pneumonitis, diffuse alveolar hemorrhage, pulmonary arterial hypertension
- Renal: Lupus nephritis, end-stage renal disease
- Hematology: Anemia of chronic disease, autoimmune hemolytic anemia, autoimmune thrombocytopenia
- Gastrointestinal: Oral ulcers, Sjogren’s syndrome, dysphagia, acute abdominal pain, abnormal liver function tests, autoimmune hepatitis
- Musculoskeletal: Arthritis, osteoporosis, fractures, asymptomatic atlantoaxial subluxation
- Infection: SLE and treatment can weaken the immune system
- Pregnancy complications: Increased risk of miscarriage, high blood pressure during pregnancy, and preterm birth
Pathophysiology
Treatment
| Drug | Indication | Anesthetic implications |
|---|---|---|
| Aspirin/NSAIDs (ibuprofen, naproxen sodium) | Antiphospholipid syndrome SLE arthritis | Peptic ulceration Platelet inhibition Renal impairment Fluid retention/electrolyte disturbance Hepatic dysfunction Bronchospasm |
| Antimalarial drugs (hydroxychloroquine) | Cutaneous SLE Pleuritis/pericarditis Arthritis Reduced renal flares | Retinotoxicity Neuromyotoxicity Cardiotoxicity |
| Corticosteroids (prednisone, methylprednisone, topical preparation) | Cutaneous SLE Nephritis Pleuritis/pericarditis Diffuse alveolar hemorrhage Neuropsychiatric SLE Mesenteric vasculitis SLE pancreatitis | Hyperglycemia Hypercholesterolemia Hypertension Osteoporosis |
| Immunosuppressants | ||
| Cyclophosphamide | Nephritis Neuropsychiatric SLE | Myelosuppression Pseudocholinesterase inhibition Cardiotoxicity Leucopenia Hemorrhagic cystitis |
| Azathioprine | Arthritis | Myelosuppression Hepatotoxicity |
| Methotrexate | Arthritis Cutaneous SLE | Myelosuppression Hepatic fibrosis/cirrhosis Pulmonary infiltrates/fibrosis |
| Mycophenolate mofetil | Nephritis Hemolytic anemia, thrombocytopenia | GI upset Pancytopenia |
Management
Preoperative management
- History: Review disease activity index, accrued organ damage, and drug history
- Examination: Thorough examination of cardiovascular, respiratory, and neurological systems, including testing for atlantoaxial subluxation symptoms and signs
- Full blood count: Test for anemia, thrombocytopenia, and leucopenia; consider further testing for hemolysis if anemia is present
- Serum electrolytes, creatinine, urea: Any abnormality requires further investigation for lupus nephritis
- Liver function tests: Abnormalities should prompt review for autoimmune or drug hepatotoxicity
- Coagulation studies: Elevated aPTT requires investigation for the presence of lupus anticoagulant
- Anti-dsDNA, complement levels: May reflect lupus activity after comparison with previous baseline measurements
- Urinalysis: Proteinuria, red cells, white cells, and cellular casts may indicate clinically silent disease and prompt further investigation
- ECG: Silent ischemia, myocarditis, pericarditis, and conduction abnormalities may be identified
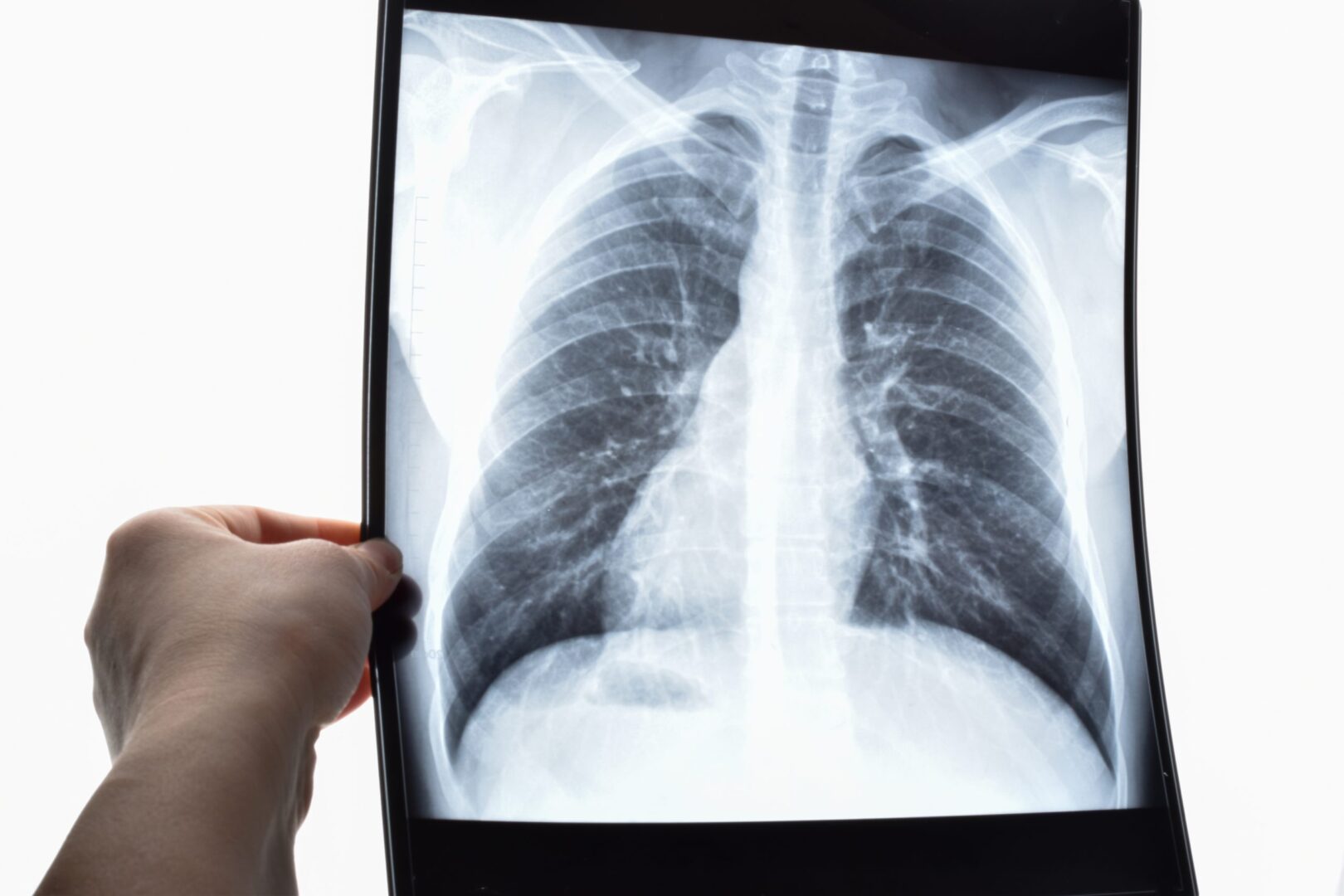
- Chest radiograph: Pleural effusion, interstitial pneumonitis, pericardial effusion, or subglottic stenosis may be seen
Intraoperative management
- 5-lead ECG: Accelerated coronary artery disease, conduction abnormalities
- Intra-arterial blood pressure monitoring: Case-dependent, consider in the presence of myocarditis, conduction abnormalities, valvular abnormalities, or autonomic dysfunction
- Laryngeal mask airway if appropriate: Minimize airway manipulation due to the risk of inflammation and post-extubation airway edema
- Difficult airway precautions with immediate access to smaller-size endotracheal tubes: Vocal cord paralysis, subglottic stenosis, or laryngeal edema may make intubation difficult
- Standard antibiotic prophylaxis: Innate susceptibility to infection and immunosuppressive therapy predispose to infection risk
- Caution with muscle relaxants: Azathioprine and cyclophosphamide may interact with muscle relaxants
- Renal protective strategies: Maintain urine output, avoid hypoperfusion and hypotensive states, and use nephrotoxic drugs cautiously due to the possibility of subclinical lupus nephritis
- Careful patient positioning: Predisposition to peripheral neuropathies and osteoporosis
- Antithrombotic prophylaxis: Institute mechanical and pharmacological measures early, especially in the presence of antiphospholipid antibodies
- Eye protection and artificial tears/lubrication: Sjogren’s syndrome may predispose to corneal abrasions despite adequate eye taping
- Temperature monitoring: Hypothermic state may induce vasospasm in patients with Raynaud’s phenomenon
- Pain management: Consider side effects of systemic analgesics; regional techniques may be helpful if neuropathies, myelitis, and coagulopathies are excluded
- Corticosteroid cover: Adrenal suppression may have resulted from long-term corticosteroid therapy with the need for a “stress dose” perioperatively
Postoperative management
- Pain management: Minimize systemic side effects
Keep in mind
- A thorough preanesthetic evaluation is mandatory for safe anesthesia
- The anesthetic plan must be individualized based on the degree of involvement of various systems, current medications, and laboratory results
Suggested reading
- Erez BM. Systemic Lupus Erythematosus: A Review for Anesthesiologists. Anesthesia & Analgesia. 2010;111(3):665-676.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com