Learning objectives
- Describe and classify traumatic brain injury
- Describe the acute management goals for traumatic brain injury patients
- Manage traumatic brain injury patients
Background
- Traumatic brain injury is the leading cause of death and disability in young adults in the developed world
- Heterogeneous condition in terms of etiology, severity, and outcome
- Can be divided into primary and secondary brain injury
- Primary injury occurs as a consequence of the initial physical insult (skull fracture, contusions, intracranial hematoma, cerebral edema, diffuse brain injury)
- Secondary injury results from inflammatory and neurotoxic processes: Increased intracranial pressure, hypoperfusion, cerebral ischemia
Classification
Glasgow Coma Scale:
- 15-13: Mild
- 13-9: Moderate
- <8: Severe
| Component | Score | |
|---|---|---|
| Eye opening | Spontaneous | 4 |
| To speech | 3 | |
| To pain | 2 | |
| None | 1 | |
| Best verbal response | Orientated | 5 |
| Confused | 4 | |
| Inappropriate | 3 | |
| Incomprehensible | 2 | |
| None | 1 | |
| Best motor response | Obeying | 6 |
| Localizing | 5 | |
| Withdrawing | 4 | |
| Flexing | 3 | |
| Extending | 2 | |
| None | 1 |
Immediate management
| System | Management goals |
|---|---|
| Airway | Early tracheal intubation if GCS≤8 or unable to maintain respiratory goals |
| Respiratory | Avoid hypoxia, maintain SaO2>97%, PaO2>11 kPa |
| Maintain a PaCO2 value of 4.5 –5.0 kPa | |
| Hyperventilation, a PaCO2 value of 4.0 – 4.5 kPa reserved for impending herniation |
|
| Cardiovascular | Avoid hypotension, maintain MAP>80 mmHg |
| Replace intravascular volume, avoid hypotonic and glucose-containing solutions | |
| Use blood as necessary, reverse existing coagulopathy | |
| Vasopressor agents as necessary to maintain CPP | |
| Brain | Monitor ICP, avoid ICP>20 mmHg |
| Maintain CPP>60 mmHg | |
| Adequate sedation and analgesia | |
| Hyperosmolar therapy, keep Na+,<155 mmol/L, Posm<320 mosm/L | |
| CSF drainage | |
| Treat seizures | |
| Barbiturate coma, decompressive craniectomy, hypothermia, all reserved for elevated ICP refractory to standard medical care |
|
| Metabolic | Monitor blood glucose, aim for blood glucose 6– 10 mmol/L |
| Avoid hyperthermia | |
| DVT thromboprophylaxis |
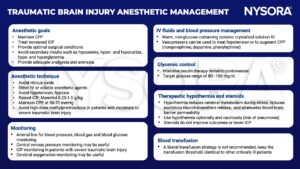
Anesthetic management
CPP, cerebral perfusion pressure; ICP, intracranial pressure
Suggested reading
- Dinsmore J. Traumatic brain injury: an evidence-based review of management. Continuing Education in Anaesthesia Critical Care & Pain. 2013;13(6):189-95.
- Curry P, Viernes D, Sharma D. Perioperative management of traumatic brain injury. Int J Crit Illn Inj Sci. 2011;1(1):27-35.
- Moppett IK. Traumatic brain injury: assessment, resuscitation and early management. Br J Anaesth. 2007;99(1):18-31.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







