Learning objectives
- Describe common causes of VAE and high-risk procedures
- Prevent VAE
- Manage VAE
Definition and mechanisms
- Venous air embolism (VAE) is caused by the ingress of gas into the venous system, most commonly air
- Rare iatrogenic complication in a wide range of clinical scenarios involving line placement, trauma, barotrauma, and several types of surgical procedures including cardiac, vascular, and neurosurgery
- Traditionally, surgery and trauma were the most significant causes of air embolism; now, endoscopy, angiography, tissue biopsy, thoracocentesis, hemodialysis, and central/peripheral venous access comprise a greater proportion
- May cause end-organ ischemia or infarction.
- May cause direct endothelial injury leading to the release of inflammatory mediators, activation of the complement cascade, and in situ thrombus formation
Signs & symptoms
- The presentation of VAE is dependent on the rate and volume of air entrained; Signs include:
- Apnea
- Hypoxia
- Cardiopulmonary collapse
- Tachypnea
- Tachycardia
- Hypotension
- Altered mental status
- Decreased conscious level
- Focal neurological deficits
- ‘Mill wheel’ murmur on cardiac auscultation
- Pulmonary edema may develop later
- Light-headedness, vertigo
- Breathing difficulties
- Shortness of breath
- Chest pain
- Sense of impending death
- ETCO2 falls
- Arterial oxygen saturation falls
- Hypoxemia
- ECG abnormalities (tachyarrhythmias, atrioventricular block, signs of right ventricular strain, ST-segment elevation or depression, non-specific T wave changes)
- Transesophageal echocardiography is the most reliable monitor to detect VAE
Prevention
- Patient positioning: avoid the sitting position and Trendelenburg position during the insertion of central venous catheters, try to prevent a negative gradient between the open site veins and the right atrium (increasing right atrial pressure via leg elevation and using the “flex” option on the operating table control)
- Holding ventilation when placing tunnel catheters
- Removal of temporary catheter synchronized with active exhalation/Valsalva maneuver or positive end-expiratory pressure
- Avoid nitrous oxide
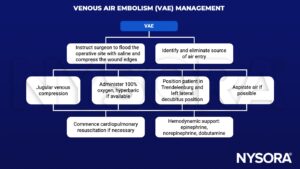
Management
Suggested reading
- Chuang DY, Sundararajan S, Sundararajan VA, Feldman DI, Xiong W. Accidental Air Embolism. Stroke. 2019;50(7):e183-e186.
- McCarthy CJ, Behravesh S, Naidu SG, Oklu R. Air Embolism: Diagnosis, Clinical Management and Outcomes. Diagnostics (Basel). 2017;7(1):5. Published 2017 Jan 17.
- Mirski MA, Lele AV, Fitzsimmons L, Toung TJ. Diagnosis and treatment of vascular air embolism. Anesthesiology. 2007;106(1):164-177.
- Webber S, Andrzejowski J, Francis G. Gas embolism in anaesthesia. BJA CEPD Reviews. 2002;2(2):53-7.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com


