Anatomical study of the obturator canal block: Insights into a precise technique for the obturator nerve block
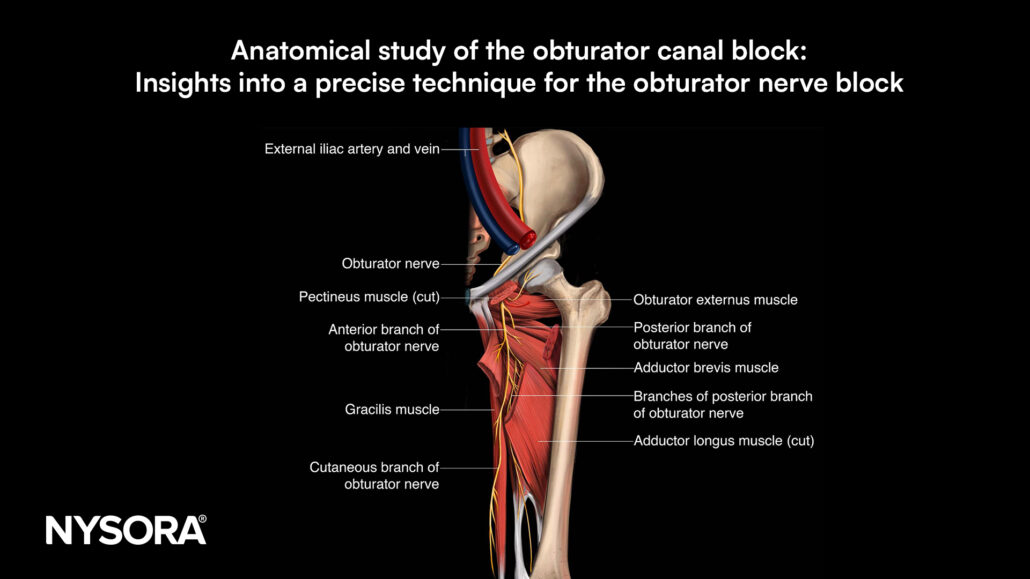
The obturator nerve (ON) plays a vital role in innervating the adductor muscles and contributing to the hip and knee joint innervation. Given its role in procedures requiring hip and knee anesthesia, the ON has become a target for nerve blocks. However, the obturator nerve’s anatomy and variations in its branching can complicate this block. Traditional methods for blocking the obturator nerve have shown varying levels of success due to these anatomical complexities. A recent anatomical study examined an ultrasound-guided approach targeting the obturator canal’s exit, aiming to clarify anatomical landmarks and solution distribution to enhance the accuracy and effectiveness of the obturator canal block (OCB).
Study objective and methods
This anatomical study sought to evaluate the distribution and effectiveness of an ultrasound-guided OCB at the exit of the obturator canal. The study used 10 cadavers to generate 20 hemipelvis samples. Ultrasound references helped identify key landmarks like the obturator canal, iliopubic ramus, pectineus, and external obturator muscles, as well as the obturator membrane.
- Injection technique: A low-frequency convex transducer initially identified the area, and a high-frequency linear transducer was then used to guide the injection of methylene blue dye at the exit of the obturator canal.
- Dissection and assessment: Dissections followed the injections to evaluate dye distribution within the obturator nerve’s branches, particularly the common trunk, anterior branch, and posterior branch.
Key findings
The study revealed consistent dye distribution across key branches of the obturator nerve, suggesting that the ultrasound-guided OCB technique provides precise coverage of the nerve and its branches.
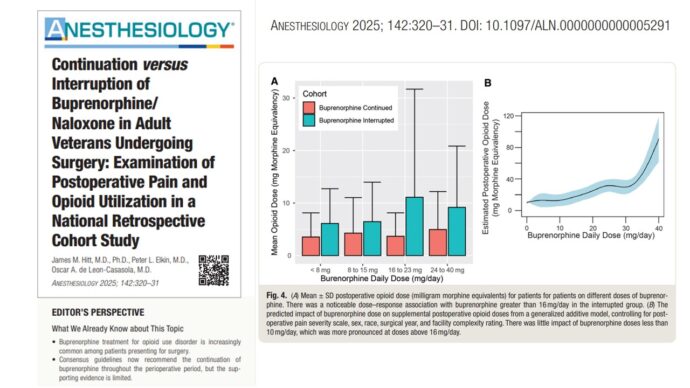
- Dye distribution: The methylene blue dye stained the common trunk and anterior branch of the obturator nerve in all samples (100%) and the posterior branch in 80% of cases. This indicates that the ultrasound-guided technique achieved comprehensive coverage of the obturator nerve at the canal exit.
- Intrapelvic staining: Intrapelvic diffusion of the dye was observed in 65% of the samples, suggesting effective solution spread from the injection site through the obturator canal and into the pelvis.
- Anatomical landmarks: The iliopubic ramus and obturator membrane were found to be crucial landmarks, allowing for accurate nerve location and injection placement.
Conclusion
The study concluded that an ultrasound-guided approach targeting the obturator canal exit provides a reliable method for the obturator nerve block, offering high coverage rates for the nerve branches. By employing clear anatomical landmarks, this technique allows for reproducibility in clinical settings, reducing the risk of missing the nerve branches, which could otherwise result in incomplete anesthesia.
Future research
Further studies are needed to confirm this technique’s clinical effectiveness and safety. Future clinical trials could explore optimal injection volumes, needle approaches, and anatomical variations to refine the method, improving anesthesia practices for hip and knee procedures requiring complete adductor muscle relaxation.
For more detailed information, refer to the full article in RAPM.
Labandeyra H, Goffin P, Riera R, Vallejo A, Prats-Galino A, Sala-Blanch X. Obturator canal block: an anatomical study. Reg Anesth Pain Med. Published online November 2, 2024.
Download the Nerve Blocks App HERE for in-depth insights on the obturator nerve block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks!