Learning objectives
- Describe antiphospholipid antibody syndrome (APS)
- Signs and symptoms and management of APS
Definition and mechanism
- Antiphospholipid syndrome (APS) or Hughes syndrome is a disorder of the immune system that creates antibodies that attack tissues in the body by mistake
- These antibodies can cause blood clots to form in arteries and veins, leading to a heart attack, stroke, and other conditions
- Can result in miscarriage and stillbirth during pregnancy
- Primary APS: the sole manifestation of an autoimmune process
- Secondary APS: in association with another disease such as systemic lupus erythematosus
- Antiphospholipid syndrome is more common in women than in men
- Causes are not completely understood and include environmental or genetic factors or an existing autoimmune disorder
- In very rare cases, blood clots can suddenly form throughout the body, resulting in multiple organ failures → catastrophic antiphospholipid syndrome (CAPS), or Asherson syndrome
- CAPS requires immediate emergency treatment with high-dose anticoagulants
Signs and symptoms
| Vascular thrombosis | Arterial thrombosis | Stroke Transient ischaemic attack Myocardial infarction Venous thrombosis |
| Venous thromboembolism | Venous thromboembolism Pulmonary embolism Small vessel thrombosis |
|
| Obstetric morbidity | ≥ 1 unexplained fetal death at or beyond week 10 of gestation ≥ 1 premature birth due to severe pre-eclampsia, eclampsia, or consequences of placental insufficiency ≥ 3 unexplained consecutive spontaneous abortions before week 10 of gestation | |
| Cardiac manifestations | Valvular heart disease Cardiomyopathies | |
| Neurological manifestations | Cognitive dysfunction Headache or migraine Multiple sclerosis Transverse myelopathy Epilepsy | |
| Dermatologic manifestations | Livedo reticularis Skin ulceration Pseudo-vasculitic lesion Distal gangrene Superficial phlebitis Malignant atrophic papulosis-like lesion Subungual splinter hemorrhage | |
| Renal manifestations | Thrombotic microangiopathy Chronic vascular damage | |
| Hematologic manifestations | Thrombocytopenia Hemolytic anemia |
Risk factors
- Pregnancy
- Immobility
- Surgery
- Smoking
- Oral contraceptives or estrogen therapy for menopause
- High cholesterol and triglyceride levels
- Systemic autoimmune diseases such as lupus
Complications
- Kidney failure
- Stroke
- Cardiovascular problems
- Pulmonary embolism
- Pregnancy complications
- Miscarriages
- Stillbirths
- Premature delivery
- Slow fetal growth
- Pre-eclampsia
Treatment
- Primary thromboprophylaxis for aPL carriers with no prior history of vascular thrombosis and/or obstetric events
- Low-dose aspirin (75-100 mg/d)
- Lifestyle changes: smoking cessation, weight loss, control of hypertension and hyperlipidemia
- A prophylactic dose of low-molecular-weight heparin (LMWH) in high-risk situations such as surgery, prolonged immobilization, and the puerperium
- Secondary thromboprophylaxis for the prevention of recurrence after thrombotic and/or obstetric events in patients with a prior history
- Previous venous thrombosis:
- Anticoagulation: target INR of 2.0-3.0
- Previous arterial thrombosis:
- High-intensity anticoagulation: target INR of 3.0-4.0 or a target INR of 2.0–3.0 combined with low-dose aspirin
- Previous venous thrombosis:
- CAPS
- Combination therapy with glucocorticoid, heparin, and plasmapheresis or IV immunoglobulin, rituximab, cyclophosphamide, or eculizumab
- Pregnant women
- Combination therapy:
- Low-dose aspirin and unfractionated heparin or LMWH
- Withdraw oral anticoagulants as soon as pregnancy is confirmed to prevent teratogenicity
- Patients without a history of thrombosis:
- Low-dose aspirin and a prophylactic dose of unfractionated heparin or LMWH are used for primary prevention
- Patients with a history of thrombotic events:
- Low-dose aspirin and a prophylactic dose of unfractionated heparin or LMWH are used for secondary prevention
- After delivery:
- Administer a prophylactic dose of LMWH for at least 6 weeks after delivery
- Start warfarin as soon as possible after bleeding is controlled
- Patients with APS who have not received any thromboprophylaxis before delivery and do not carry any risk factors for thrombosis, require LMWH for only 7 days following delivery
- Combination therapy:
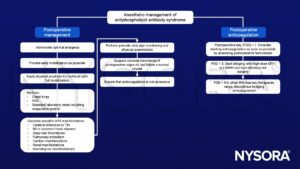
Management

Suggested reading
- Kim JW, Kim TW, Ryu KH, Park SG, Jeong CY, Park DH. Anaesthetic considerations for patients with antiphospholipid syndrome undergoing non-cardiac surgery. J Int Med Res. 2020;48(1):300060519896889.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com