Learning objectives
- Define and describe autonomic dysreflexia
- Recognize signs and symptoms of autonomic dysreflexia
- Manage patients with autonomic dysreflexia
Definition & mechanisms
- Autonomic dysreflexia is a condition that emerges after a spinal cord injury, usually when the damage has occurred above the T6 level
- Dysregulation of the autonomic nervous system leads to an uncoordinated sympathetic response that may result in a potentially life-threatening hypertensive episode when there is a noxious stimulus below the level of the spinal cord injury
- Noxious stimuli consist usually of bladder or bowel distension
- The higher the injury, the greater the severity of the cardiovascular dysfunction
- Significantly increased risk of stroke by 300% to 400%
Signs & symptoms
- Severe headache
- Hypertension
- Piloerection above the level of injury
- Bradycardia
- Facial flushing
- Pallor
- Cold skin
- Sweating in the lower part of the body
- Visual disturbances
- Constricted pupils
- Nasal stuffiness
- Anxiety or feelings of doom
- Nausea and vomiting
- Dizziness
Evaluation
- Identify patients at risk (injury above T6)
- Document baseline blood pressure
- When severe headache occurs, measure blood pressure
- A systolic blood pressure >150 mmHg or >40 mmHg above baseline is indicative of autonomic dysreflexia
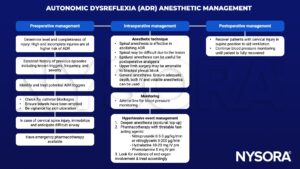
Anesthetic management
Suggested reading
- Allen KJ, Leslie SW. Autonomic Dysreflexia. [Updated 2022 Nov 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Petsas A, Drake J. Perioperative management for patients with a chronic spinal cord injury. BJA Education. 2015;15(3):123-30.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com