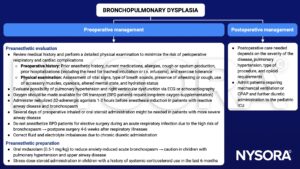
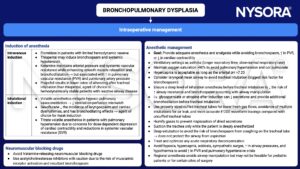
Learning objectives
- Describe bronchopulmonary dysplasia
- Understand the pathophysiology of bronchopulmonary dysplasia
- Recognize the risk factors for developing bronchopulmonary dysplasia
- Anesthetic management of a pediatric patient with bronchopulmonary dysplasia
Definition and mechanisms
- Bronchopulmonary dysplasia (BPD) is a chronic lung disease in which premature infants require long-term oxygen because the alveoli that are present, are not mature enough to function properly
- Babies are not born with BPD, the condition results from damage to the lungs, usually caused by mechanical ventilation and long-term use of oxygen
- BPD is more common in infants with a low birth weight and those who receive prolonged mechanical ventilation to treat respiratory distress syndrome
- BPD develops most commonly in the first 4 weeks after birth
| Criteria for BPD diagnosis | |
|---|---|
| Infants requiring supplemental oxygen at 28 days are diagnosed, via an assessment at 36 weeks postmenstrual age, as having: | |
| Mild BPD | Infant breathing room air |
| Moderate BPD | Infant requiring <30% FiO2 |
| Severe BPD | Infant requiring >30% FiO2 or positive pressure ventilation |
Signs and symptoms
- Hypoxemia
- Hypercapnia
- Crackles, wheezing, and decreased breath sounds
- Increased bronchial secretions
- Hyperinflation
- Feeding problems due to prolonged intubation (oral-tactile hypersensitivity/oral aversion)
- Need for continued oxygen therapy after the gestational age of 36 weeks
- Repeated lower respiratory infections that may require hospitalization
- Delayed growth and development
Causes
Risk factors
- Antenatal factors
- Prematurity
- Postnatal factors
- Mechanical ventilation
- Sepsis
- Oxygen toxicity
- Patent ductus arteriosus
Complications
- Airway disease and respiratory morbidity due to prolonged tracheal intubation and mechanical ventilation
- Development of tracheomalacia and bronchomalacia
- BPD spells: Acute cyanotic events caused by increases in central airway compliance
- Subglottic stenosis
- Airway granulomas
- Pseudopolyps
- Persistent airway obstruction and hyperreactivity
- Pulmonary hypertension
- Cor pulmonale
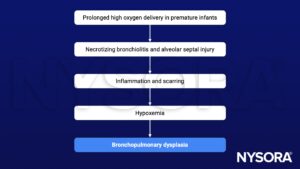
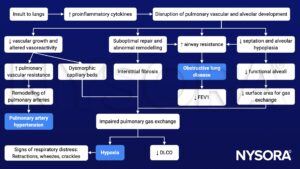
Pathophysiology
Treatment
- There is no cure for BPD, treatment focuses on minimizing further lung damage and providing support for the infant’s lungs
- Oxygen therapy
- Nasal continuous positive airway pressure (NCPAP)
- Bilevel positive airway pressure (BiPAP)
- Medications
- Diuretics: Decrease fluid in and around the alveoli
- Bronchodilators: Relax the muscles around the air passages, widening the airway openings and making breathing easier
- Corticosteroids: Reduce and/or prevent inflammation within the lungs, reduce swelling in the trachea, and decrease the mucus production
- Viral immunization: Prevent infection (i.e., respiratory syncytial virus)
Management
Prevention
- Antenatal steroid administration
- Surfactant therapy
- Improved ventilator strategies to minimize lung injury
Keep in mind
- BPD is one of the most common pulmonary disorders encountered by pediatric anesthesiologists
- BPD, a common sequala of preterm birth, is associated with persistent airway disease and pulmonary hypertension
- Anesthetic effects might have life-threatening consequences in BPD patients (limited respiratory reserve)
- Intraoperative bronchospasms or airway collapse → hypoxemia, acute pulmonary hypertension, right-sided heart failure, arrhythmias, and death
- Effects on myocardial contractility can impair right ventricular function → reduction in cardiac output and cardiovascular compromise → cor pulmonale
- Respiratory infections (i.e., pneumonia) can further complicate the perioperative course
Suggested reading
- Lauer R, Vadi M, Mason L. Anaesthetic management of the child with co-existing pulmonary disease. BJA. 2012;109(1):i47-i59.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com