Case study: Carpal tunnel release
Case presentation
A 45-year-old female patient with a confirmed diagnosis of carpal tunnel syndrome in the right hand was scheduled for elective carpal tunnel release surgery. The patient experienced significant pain, numbness, and tingling in the affected hand, affecting daily activities and quality of life. As part of the comprehensive pain management plan, an ultrasound-guided wrist block was proposed to provide localized anesthesia and minimize postoperative pain.
Nerve block technique
The wrist block technique consists of a mid-forearm level block of the median and ulnar nerves, followed by a subcutaneous infiltration of the local anesthetic at the wrist crease for any remaining cutaneous branches of the musculocutaneous, radial, or ulnar nerves.
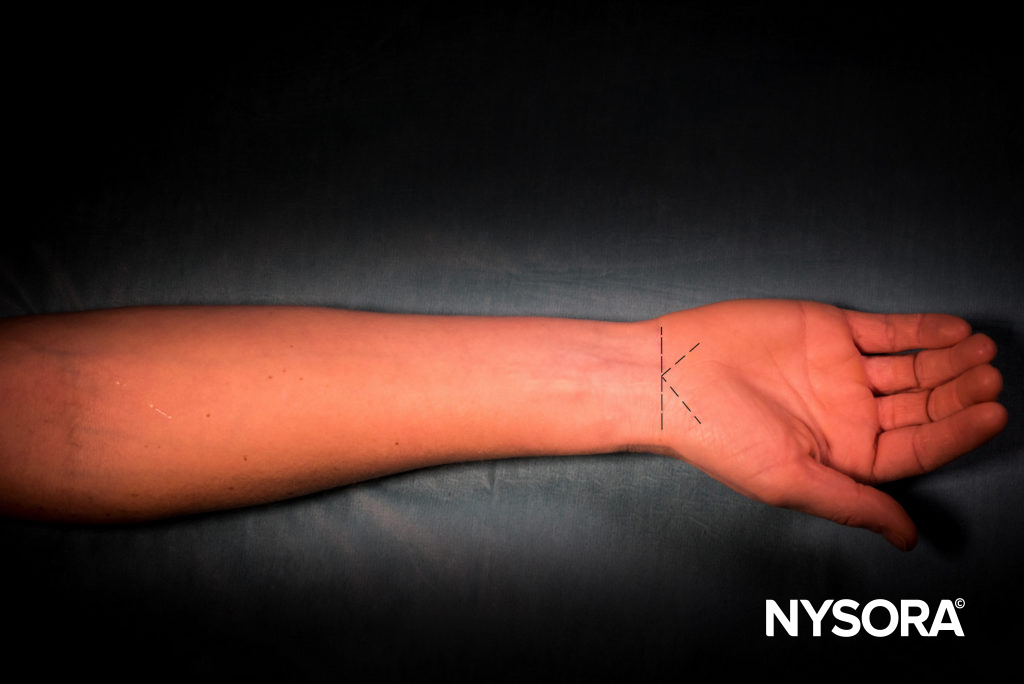
Subcutaneous infiltration.
Under ultrasound guidance, the median and ulnar nerves were identified between the superficial and deep flexors of the wrist and fingers.
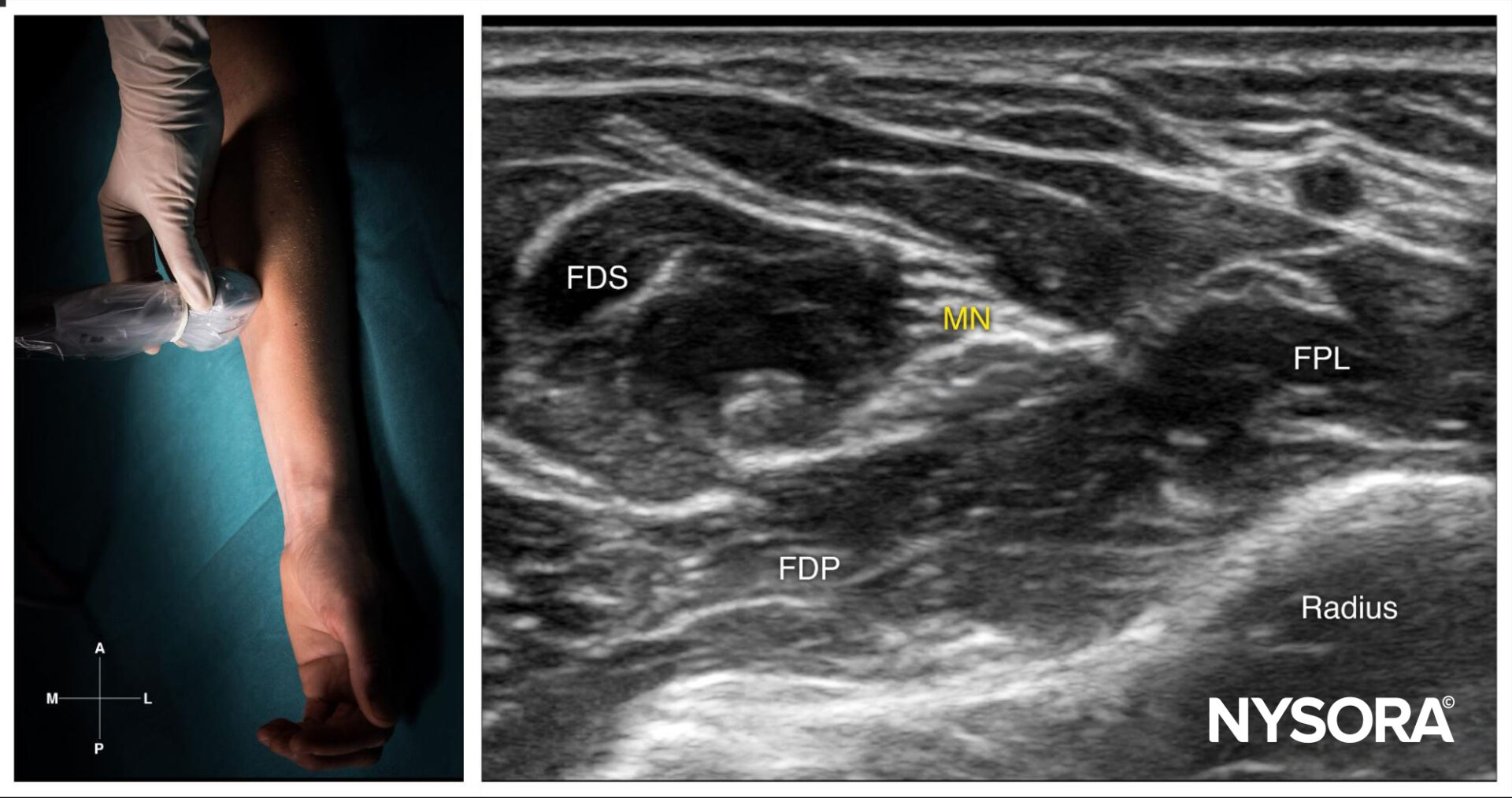
Median nerve block at the level of the wrist; transducer position and sonoanatomy. MN, median nerve; FPL, flexor pollicis longus muscle; FDS, flexor digitorum superficialis muscle; FDP, flexor digitorum profundus muscle.
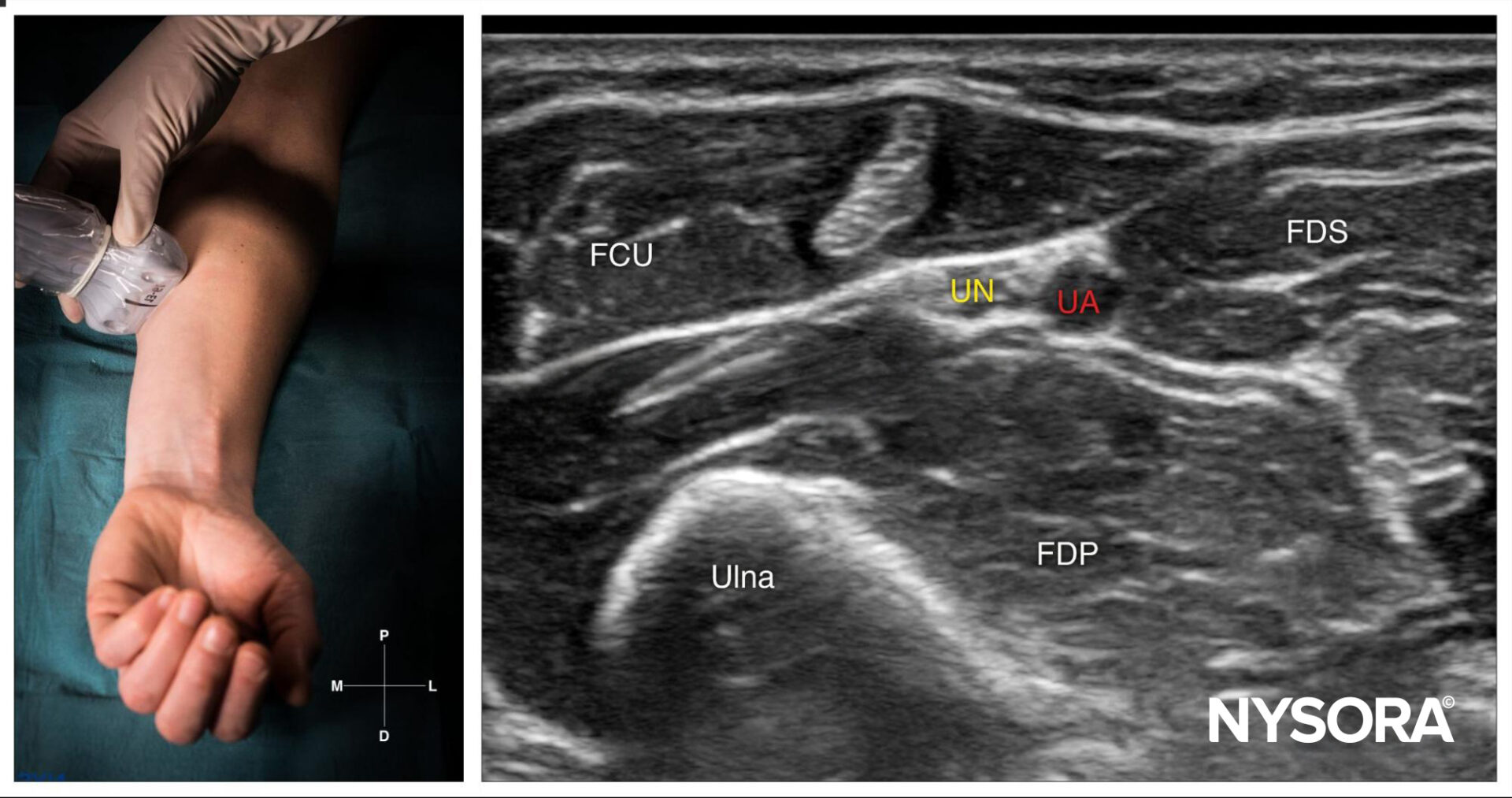
Ulnar nerve block at the level of the wrist; transducer position and sonoanatomy. UN, ulnar nerve; UA, ulnar artery; FCU, flexor carpi ulnaris; FDP, flexor digitorum profundus muscle; FDS, flexor digitorum superficialis muscle.
A 25-gauge needle was then inserted in-plane or out-of-plane and 4 mL of lidocaine 2% was injected into the fascia containing the nerves. The onset of anesthesia was observed within 10 minutes.
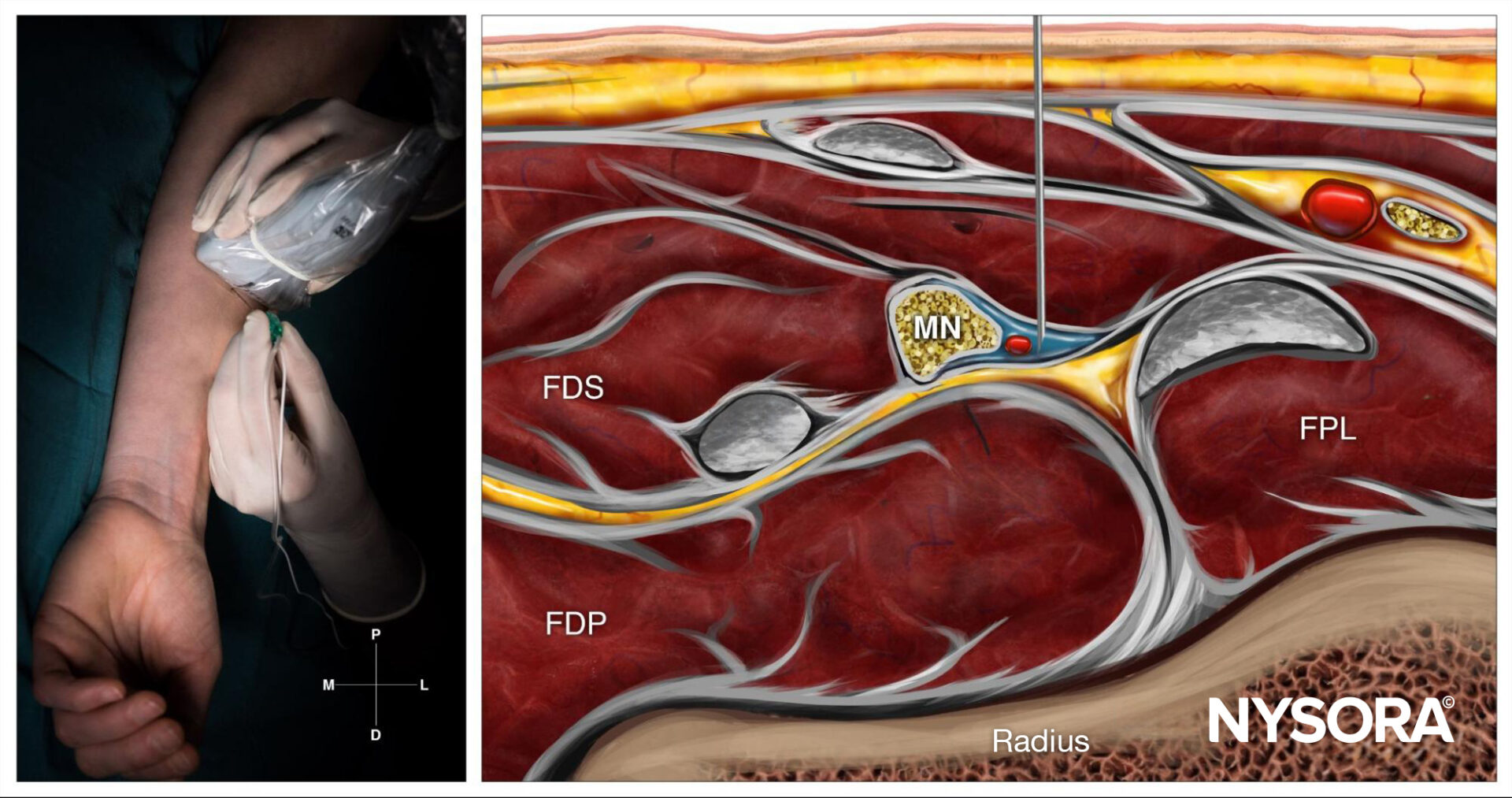
Median nerve block at the level of the wrist; Reverse Ultrasound Anatomy with needle insertion out-of-plane and local anesthetic spread (blue). MN, median nerve; FPL, flexor pollicis longus muscle; FDS, flexor digitorum superficialis muscle; FDP, flexor digitorum profundus muscle.
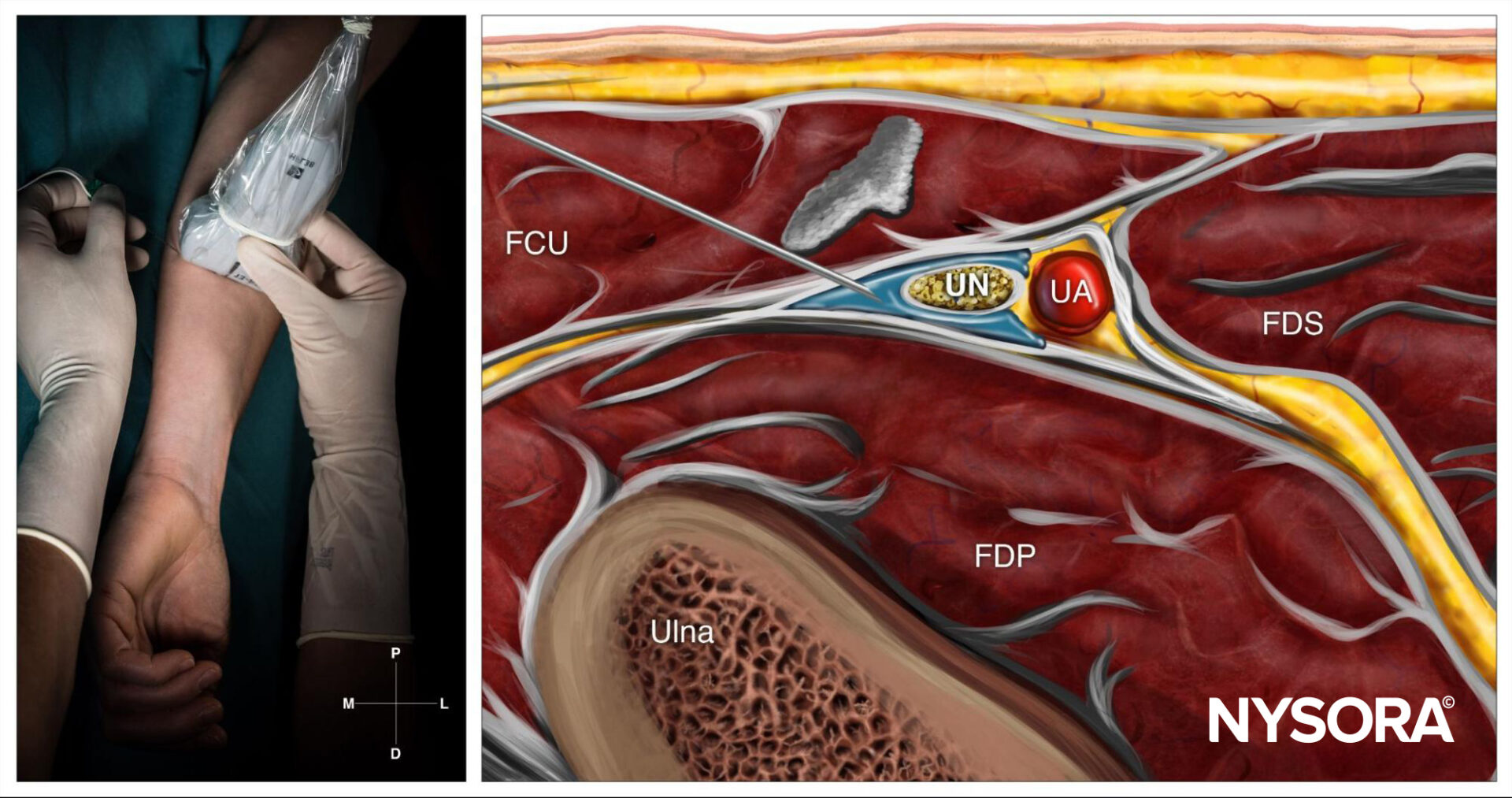
Ulnar nerve block at the level of the wrist; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). UN, ulnar nerve; UA, ulnar artery; FCU, flexor carpi ulnaris; FDP, flexor digitorum profundus muscle; FDS, flexor digitorum superficialis muscle.
Patient outcome
Following the ultrasound-guided wrist block, the patient reported immediate relief of pain and paresthesia in the affected hand. After surgery, the patient’s hand function improved, allowing for early mobilization and participation in rehabilitation exercises. The need for systemic opioids was minimized, thereby reducing the risk of associated side effects. The patient did not experience any complications or adverse events related to the wrist block.
Comparing lidocaine 2% and bupivacaine 0.5% in ultrasound-guided wrist blocks
Wrist blocks are commonly used for hand and wrist surgeries. Selecting the right local anesthetic is crucial for balancing the onset speed and duration of the block. Historically, lidocaine has been favored for its rapid onset, while bupivacaine is chosen for its prolonged duration. However, the precision ultrasound guidance offers raises questions about these traditional choices. the recent study by Van Boxstael et al. 2022 offers valuable insights into the clinical applications of these agents as this study explored the comparative efficacy of lidocaine and bupivacaine in the ultrasound-guided median and ulnar nerve blocks.
Study design
The study included 36 participants undergoing carpal tunnel release surgery. These participants were divided into four groups:
- Lidocaine 2% (Single Injection)
- Lidocaine 2% (Dual Injection)
- Bupivacaine 0.5% (Single Injection)
- Bupivacaine 0.5% (Dual Injection)
Ultrasound guidance was used for all procedures, ensuring precise anesthetic delivery.
Key outcome measures were:
- Onset time of sensory blockade
- Duration of sensory blockade
Findings
- Onset time:
- The onset of sensory block was similar across all groups, with no statistically significant differences between lidocaine and bupivacaine or between single and dual injections.
- Average onset times:
- Lidocaine: 9.2 ± 3.4 minutes
- Bupivacaine: 9.5 ± 3.1 minutes
- Duration:
- Bupivacaine provided significantly longer sensory block duration compared to lidocaine:
- Bupivacaine: 27.3 ± 11.6 hours
- Lidocaine: 8.4 ± 4.1 hours
- There was no significant difference in block duration between single and dual injections.
- Bupivacaine provided significantly longer sensory block duration compared to lidocaine:
- Efficacy of dual injections:
- Adding a second injection site along the nerve pathway did not enhance the onset or duration of the block.
Implications for clinical practice
- Anesthetic choice based on duration:
- For surgeries requiring extended postoperative analgesia, bupivacaine 0.5% is the superior choice. Lidocaine, with its shorter duration, may be more suitable for shorter procedures.
- Single injection sufficiency:
- When performed with ultrasound guidance, a single injection achieves optimal results without additional injections.
- Challenging traditional practices:
- The findings question the need to mix anesthetics to achieve rapid onset and prolonged duration. Under ultrasound guidance, bupivacaine alone suffices for both needs.
Conclusion
This study redefines the approach to ultrasound-guided wrist blocks. The data suggests that the choice of local anesthetic should prioritize block duration over onset speed, given the similar onset times of lidocaine and bupivacaine. Furthermore, the absence of added benefits from dual injections simplifies procedural protocols, enhancing efficiency in clinical settings.
For more information, refer to the article in Anesthesia & Analgesia.
Van Boxstael, Sam MD*,†; Lopez, Ana M. MD, PhD*; Balocco, Angela Lucia MD*; Vandepitte, Catherine MD, PhD*; Meex, Ingrid PhD*; Duerinckx, Joris MD‡; Kuroda, Maxine M. PhD*; Mesotten, Dieter MD, PhD*,†; Van Herreweghe, Imre MD*; Hadzic, Admir MD, PhD*. Effect of Lidocaine 2% Versus Bupivacaine 0.5% and 1 Versus 2 Dual Separate Injections on Onset and Duration of Ultrasound-Guided Wrist Blocks: A Blinded 2 × 2 Factorial Randomized Clinical Trial. Anesthesia & Analgesia 134(6):p 1318-1325, June 2022.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!