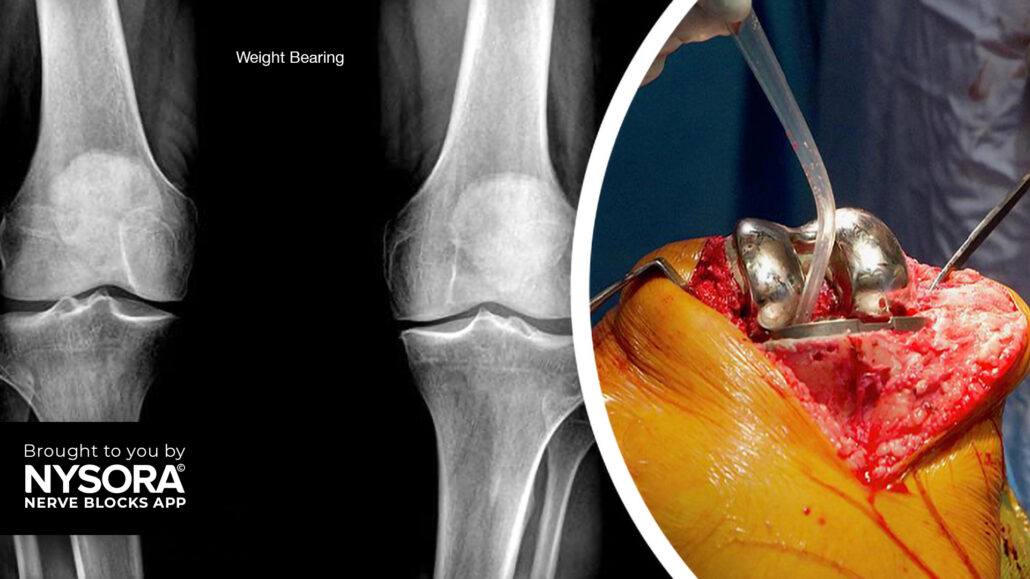
Case study: Total knee arthroplasty
Case presentation
A 65-year-old male patient with severe osteoarthritis of the right knee was scheduled for elective total knee arthroplasty. The patient had a history of chronic knee pain and limited mobility and was keen on exploring options for effective pain relief. As part of the comprehensive pain management plan, an ultrasound-guided femoral nerve block was planned to provide targeted analgesia for improved pain control.
Nerve block technique
The patient was positioned supine with the lower extremity fully extended and slightly rotated externally. A high-frequency linear transducer was placed in a transverse orientation over the femoral crease to identify the femoral nerve.
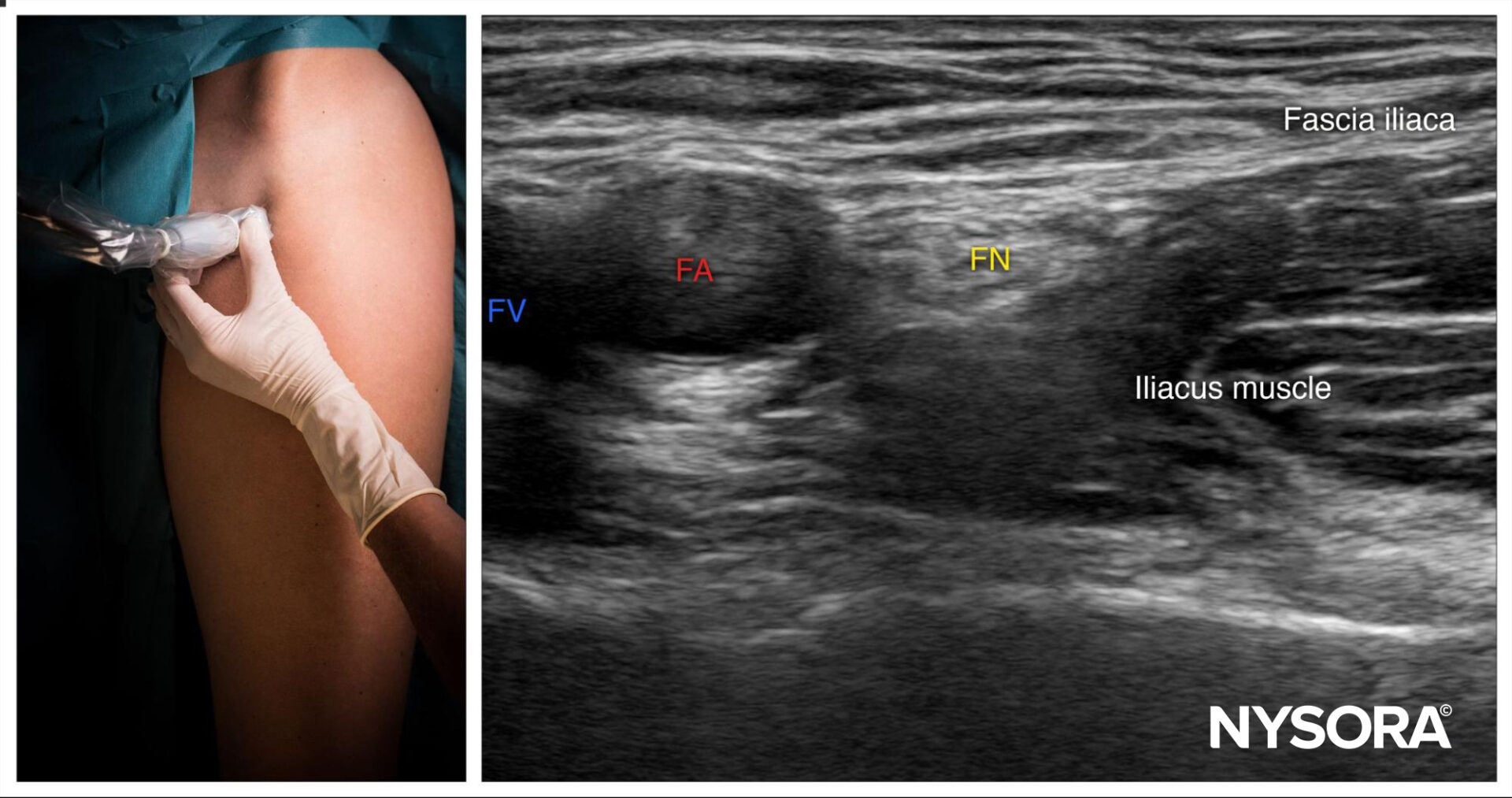
Femoral nerve block; transducer position and sonoanatomy. FA, femoral artery; FV, femoral vein; FN, femoral nerve.
A 22-gauge needle was inserted in-plane, in a lateral-to-medial direction, to pierce the fascia iliaca lateral to the femoral nerve. A total of 12 mL of bupivacaine 0.5% was injected ensuring proper spread around the femoral nerve.
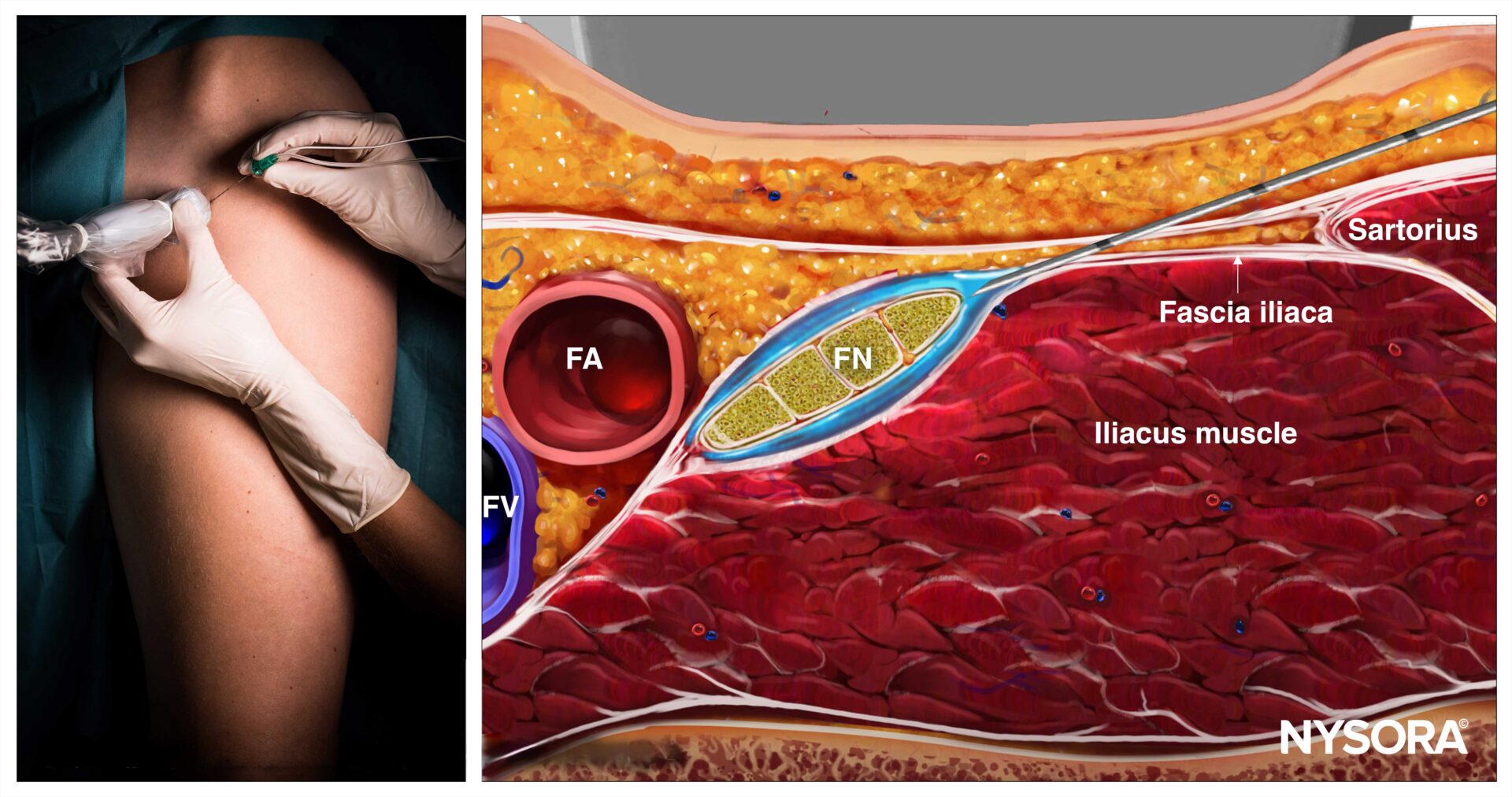
Femoral nerve block; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). FA, femoral artery; FV, femoral vein; FN, femoral nerve.
Patient outcome
Following the ultrasound-guided femoral nerve block, the patient experienced significant pain relief within minutes. The patient reported improved comfort, allowing for early mobilization and participation in physical therapy. The need for systemic opioids was greatly reduced, thereby minimizing associated side effects such as sedation and nausea. The patient did not experience any immediate or delayed complications related to the nerve block.
Enhancing postoperative pain management in total knee arthroplasty: the role of tibial nerve blocks
In the evolving field of orthopedic surgery, pain management remains a critical challenge, especially in procedures like total knee arthroplasty (TKA). A study published in the Journal of Clinical Medicine by Mira-Puerto et al. 2024 investigates adding a tibial nerve block to the femoral nerve block for managing postoperative pain in TKA patients. This innovative approach not only highlights the potential for improved pain control but also underscores the broader implications for reducing opioid use.
Study design
- Participants: 60 patients undergoing TKA, split evenly into an experimental group (EG) and a control group (CG).
- Interventions:
- EG: Femoral and tibial nerve blocks with neuraxial anesthesia.
- CG: Femoral nerve block with intravenous opioids and NSAIDs via an elastomeric pump.
- Evaluation Metrics: Postoperative pain scores using the Numerical Pain Rating Scale (NPRS), need for rescue analgesia, and opioid consumption within 48 hours after surgery.
Outcomes
- Pain scores:
- At rest, pain scores were similar between groups. However, during movement, the EG consistently reported lower NPRS values at 24, 36, and 48 hours post-surgery, with statistically significant differences observed at 48 hours.
- Rescue analgesia:
- Fewer patients in the EG required rescue analgesia compared to the CG at all time points:
- At 24 hours: 33.3% (EG) vs. 80% (CG).
- At 48 hours: No patients in the EG required rescue analgesia, compared to 10% in the CG.
- Fewer patients in the EG required rescue analgesia compared to the CG at all time points:
- Opioid consumption:
- The EG had significantly reduced opioid use. Only 33.3% of EG patients required opioids, with an average dose of 40 mg ± 62.14, compared to 100% opioid use in the CG, with an average dose of 300 mg.
- Probability of rescue analgesia:
- Kaplan-Meier survival analysis revealed that patients in the CG were more likely to require rescue analgesia at all intervals, highlighting the efficacy of the dual nerve block approach.
Advantages of adding tibial nerve blocks
- Enhanced pain control: Lower NPRS scores during movement indicate that tibial nerve blocks improve postoperative mobility and comfort.
- Reduced opioid dependence: The substantial decrease in opioid consumption aligns with current efforts to mitigate opioid-related side effects and dependency risks.
- Lower Rescue Analgesia Rates: The reduction in additional analgesic requirements underscores the effectiveness of this combined block technique.
Broader impact on patient care
- Faster rehabilitation: Improved pain management can expedite physiotherapy and recovery timelines, enhancing surgical outcomes.
- Cost-effectiveness: Reducing the reliance on opioids and additional analgesics may lower postoperative care costs.
- Patient satisfaction: Minimizing pain and adverse drug effects improves patient satisfaction and experience.
Conclusion
Adding a tibial nerve block to the femoral nerve block for TKA patients represents a promising advancement in postoperative pain management. By providing effective pain relief, reducing opioid consumption, and decreasing the need for rescue analgesia, this approach addresses both patient and systemic healthcare challenges. As surgical techniques and pain management strategies continue to evolve, this study underscores the importance of leveraging innovative interventions to enhance patient outcomes.
For more information, refer to the article in the Journal of Clinical Medicine.
Mira-Puerto A, Romero-Aroca P, Rodríguez-Gangoso A, Ferrando-de Jorge A, Duart-Oltra M, Sala-Francino P, Martínez-Segovia MC, Baget-Bernaldiz M. Evaluation of Postoperative Pain When Adding a Tibial Nerve Block to the Femoral Nerve Block for Total Knee Arthroplasty. J Clin Med. 2024 Jul 26;13(15):4387.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!