
Case study: Total shoulder arthroplasty
A 52-year-old patient with end-stage shoulder osteoarthritis was scheduled for total shoulder arthroplasty.
Total shoulder replacement can be done with interscalene brachial plexus block (ISB) alone or in combination with general anesthesia (GA). General anesthesia is more often used in patients who are having shoulder surgery in a position different than a supine position, or beach chair position. The choice of anesthetic technique – ISB alone or GA – should take
into account the patient’s preferences as well as the workflow of the individual practice, anesthesiologist, and surgeon. When used for analgesia only, interscalene brachial plexus block can be accomplished with only a few mL of local anesthetic, typically bupivacaine with or without epinephrine, and liposomal bupivacaine, where available. The latter combination provides 48 hours +1 analgesia which could be ideal for outpatient surgery, instead of perineural catheters.
When interscalene brachial plexus block is used as the sole anesthetic and analgesic technique, more local anesthetic volume and dose are needed. For surgical anesthesia, we use 10-15 mL of .5% bupivacaine. When admixing liposomal bupivacaine (Exparel®) for postoperative analgesia, we typically mix with 5 mL (analgesia) or 10 mL anesthesia) of bupivacaine 0.5%.
In a very informative publication in anesthesiology, Vandepitte et al. reported that the success rate of ISB for surgery increases sharply from approximately 57% at 6 mL to 100% at 7 mL, indicating that a small increase in the volume of ropivacaine 0.75% markedly affects the success rate. Seven mL of 0.75% ropivacaine results in successful anesthesia within 30 min, yielding an ED95 of 7 mL (95% CI 6.8-7.2).
For the group as a whole, the median (min-max) sensory block onset time was 5 (5-20) min, the median (min-max) motor blocks for the biceps and the deltoid muscles were 7.5 (5-15) min and 10 (5-15) min, respectively. However, the median (min-max) block duration was 8.9 (3-15) h, which is why we nowadays use bupivacaine instead of ropivacaine. (Vandepitte C, Gautier P, Xu D, Salviz EA, et al. Effective volume of ropivacaine 0.75% through a catheter required for interscalene brachial plexus blockade. Anesthesiology. 2013 Apr;118(4):863-7).
Check out the Interscalene Brachial Plexus Block on NYSORA’s Nerve Blocks App to learn more about this technique!

Sonoanatomy
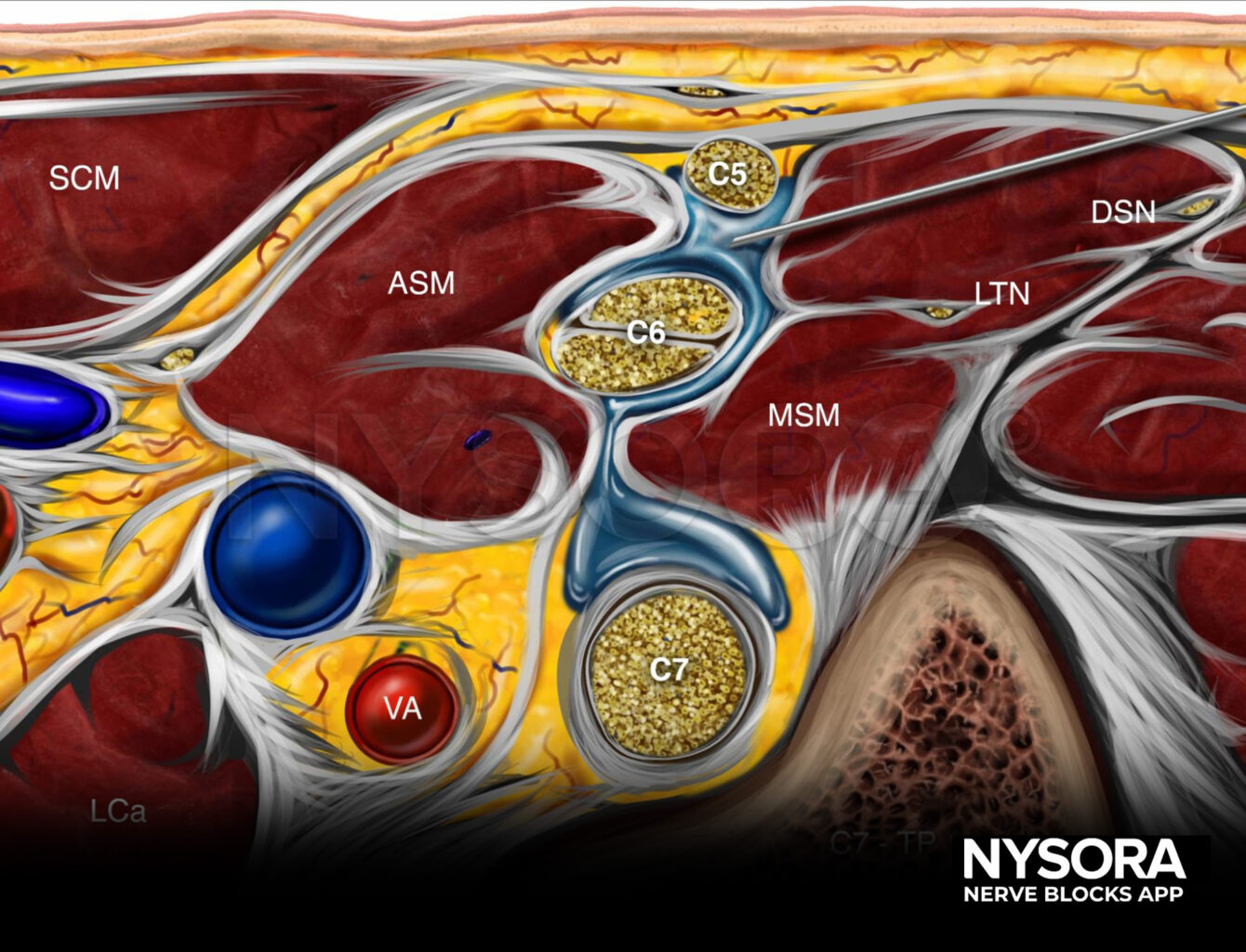
Reverse Ultrasound Anatomy
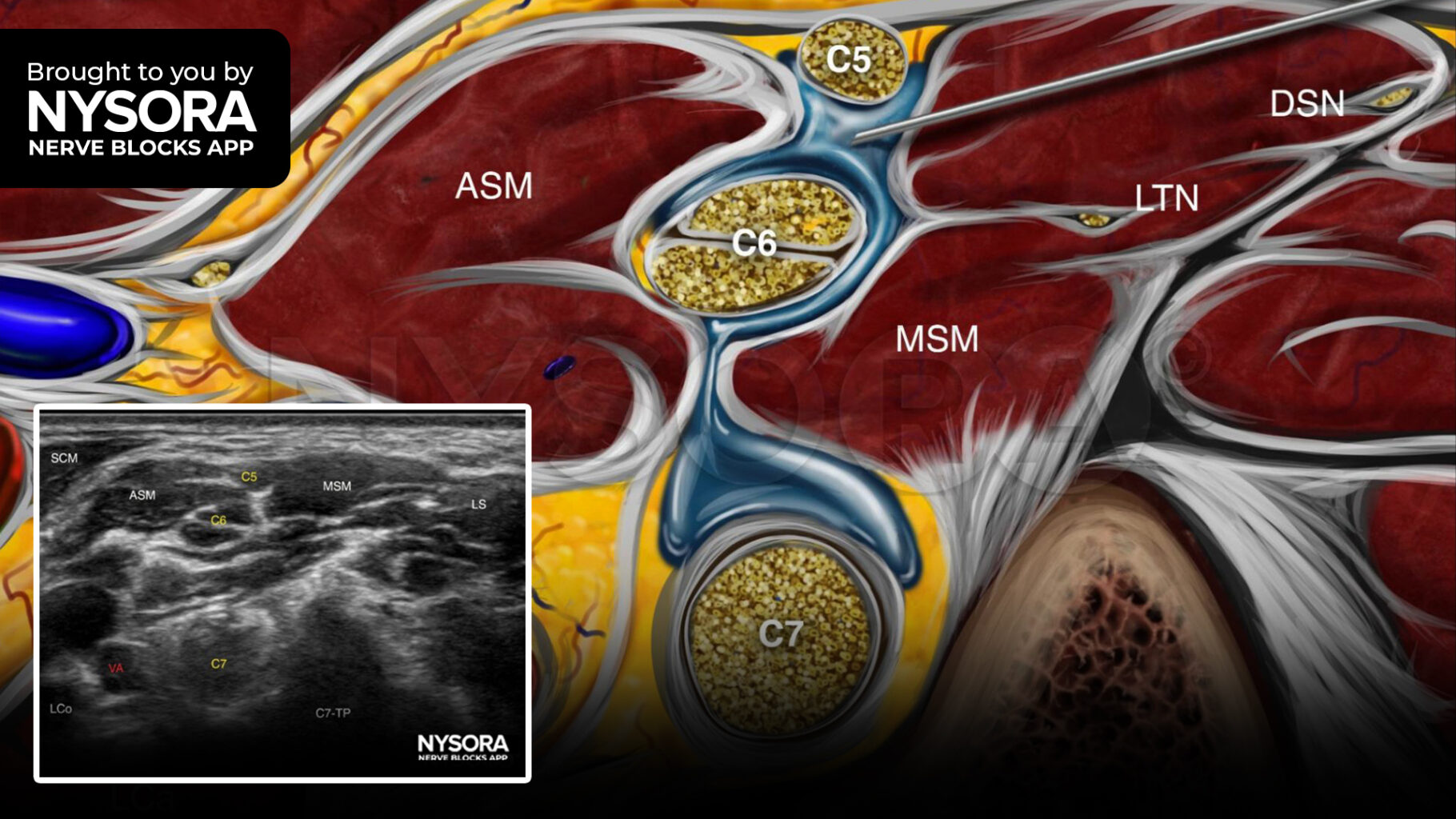
Comparison of sonoanatomy and reverse ultrasound anatomy for an interscalene brachial plexus block with needle insertion in-plane. The local anesthetic spread is shown in blue.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!
Join the discussion
We would love to hear what anesthetic you do for major shoulder surgery in your practice – and which local anesthetic, doses, mixtures and you use for analgesia. Join NYSORALMS, the community of 12,000 medical professionals, and join the conversation. It is an interactive, free-to-access community of medical experts from across the globe. This lets us create an incredible, professional, uncensored dialogue via the activity feed.



