Case study: Trigger finger – Injection
A 57-year-old woman presents with a history of chronic pain over the base of the right middle finger for four months. The patient does not have any significant comorbidities or medical conditions, including no history of rheumatoid arthritis or diabetes. She has not undergone any recent surgeries or sustained any trauma to her right hand or finger. She reports no previous episodes of similar finger pain in the past.
Physical examination
- Chronic pain over the base of the right middle finger
- No visible swelling, redness, or deformity
- No inciting factors for trigger finger were identified
Ultrasound findings
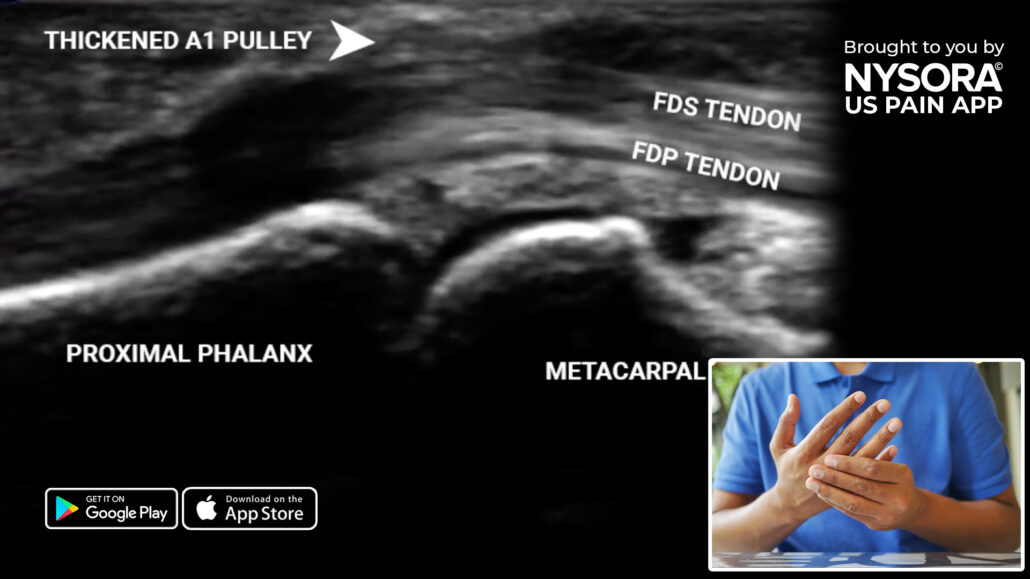
- Thickened A1 pulley: The thickened A1 pulley restricts the gliding of the flexor digitorum superficialis (FDS) tendon, but not the flexor digitorum profundus (FDP) tendon
Long-axis view of the A1 pulley at the level of the metacarpal.
Severity grading
Green’s classification is used to assess the severity of trigger finger symptoms:
- Grade I: Pain/history of catching
- Grade II: Demonstrable catching, but can actively extend the digit
- Grade III: Demonstrable locking, requiring passive extension
- Grade IV: Fixed flexion contracture
Diagnosis
The patient was diagnosed with grade II trigger finger. Trigger finger, also known as stenosing tenosynovitis, is a condition that affects the fingers and thumb, resulting in temporary locking or catching of the affected digit in a flexed position. It is characterized by pain, stiffness, and a popping or clicking sensation when attempting to straighten or bend the affected finger.
To read more about the treatment, patient outcome, and other case studies, download the most practical app on ultrasound-guided chronic pain blocks for the management of chronic pain HERE.



